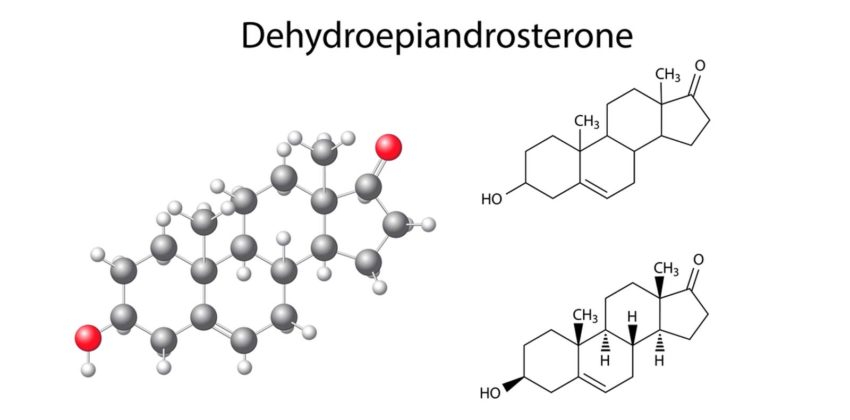
When people hear the word “hormones,” the first thing that usually pops into their minds are the primary sex hormones, such as testosterone and estrogen, and how they drive a lot of what we do on a daily basis. However, not all hormones come from the reproductive systems of men and women. In fact, the adrenal glands also produce a very useful hormone called DHEA.
What is DHEA?
DHEA, which is synthesized from cholesterol, is mainly produced by the adrenal glands, and also happens to be the steroid hormone we have the largest amounts of in our bodies. It is often referred to as the master, parent, or mother hormone because it is necessary for the creation of other hormones, such as progesterone, estrogen, and testosterone—that is to say, DHEA is converted into all these other hormones, and the biological benefits you can reap are a result of the conversion process itself.
What Can It Do?
It has been linked to a number of benefits, including the following:
- Increasing energy levels
- Decreasing feelings of fatigue
- Developing and toning muscles
|
- Building endurance and strength
- Lessening the amount of fat in the body
|
How Can You Get It?
This hormone can be obtained without a prescription from your primary physician. However, you must not settle for a brand just because it has the lowest price tag. High quality supplements may be more expensive, and you may be able to buy generics for things like painkillers and vitamins, but going for cheaper options when it comes to hormone supplements does not exactly lead to the same results. Not only could there be a chance that you are going to get more filler ingredients instead of pure DHEA, but this decision could also expose you to certain health risks due to uncertainty regarding how the product was made. You may not be able to find out if there are any toxins in it due to mishandling by the manufacturer, or if it was produced in a sanitary environment.
Another option you can consider is to undergo bioidentical hormone therapy replacement (BHRT) at a reputable institute in your area. An experienced physician can give you a proper diagnosis as well as provide you with the right nutrition, exercise, and supplement program to help rebalance your hormones. Why go for BHRT instead of the procedures that make use of synthetic hormones? The advantage of bioidentical hormones is that they have a very similar molecular make-up to the hormones that are naturally released within our bodies. This means that, because the bioidentical hormones are not too different from natural ones, the body can more efficiently synthesize these kinds of hormones.
Taking Advantage of DHEA
Besides the sources listed above, you can also obtain DHEA by eating food items that contain high amounts of healthy fats, particularly omega 3 fatty acids. Regardless of how you choose to obtain them, taking advantage of them now rather than later would be a smart decision for anybody of any age.