Peptides
- 5-amino-1MQ
- Aminophylline
- Aniracetam
- ARA 290
- Argireline + Leuphasyl
- BPC-157
- Bremelanotide
- Cerebrolysin
- CJC-1295
- Delta Sleep-Inducing Peptide
- Dihexa
- Elampretide (SS-31)
- Epithalon
- FG Loop Peptide (FGL)
- GHK-Cu
- Ginsenoside Rg3
- Glycyrrhetinic Acid
- Ipamorelin
- Kisspeptin
- KPV
- LL-37
- Melanotan 1
- Melanotan 2
- Mitochondrial ORF of the twelve S c (MOTS-c)
- MK-677 (IBUTAMOREN)
- Nicotinamide Adenine Dinucleotide (NAD+)
- Nicotinamide Riboside
- NMN (Nicotinamide Mononucleotide)
- Noopept
- Pegylated Mechano Growth Factor
- Selank
- Semax
- Sermorelin
- SRT2104
- Tesamorelin
- Thymosin Alpha 1
- Thymosin Beta 4
- Tiger 17
- Valproic Acid
- Valproic acid + PTD-DBM
- Vasoactive Intestinal Peptide
- Zinc-Thymulin
Overall Health Benefits of Thymosin Alpha 1
Thymosin Alpha 1 offers broad health benefits by enhancing immune system function, regulating inflammation, and promoting immune balance. Its therapeutic potential spans various conditions, including chronic infections, autoimmune diseases, and cancer, while supporting overall immune resilience.
- Eradicates bacteria, viruses, and fungi [1-5]
- Boosts the function of certain immune cells [6-17]
- Suppresses cancer and tumor growth [18-34]
- Accelerates the wound healing process [3, 35-38]
- Fights inflammation [39-49]
- Increases vaccine effectiveness [50-53]
Key Takeaways
- Immune Modulation: Thymosin Alpha 1 enhances the immune system by stimulating T-cells and natural killer cells, improving the body’s defense against infections and tumors.
- Anti-inflammatory Properties: It helps regulate inflammation, making it effective in conditions such as sepsis, chronic infections, and autoimmune diseases.
- Cancer Therapy Support: Thymosin Alpha 1 shows promise in cancer treatment by boosting tumor antigen recognition and enhancing the efficacy of immunotherapies.
- Infection Management: It is used in managing chronic infections, including hepatitis B, hepatitis C, and human immunodeficiency virus (HIV), improving patient outcomes.
- Safety and Tolerability: With a strong safety profile, Thymosin Alpha 1 is well-tolerated, making it suitable for long-term use in diverse clinical settings.
What is Thymosin Alpha 1?
Thymosin alpha 1 (Tα1) is a peptide that is naturally produced by the thymus gland, an essential organ for immune system development. It plays an integral role in the maturation of immune system cells known as T-cells, which are developed and regulated within the thymus gland to fight harmful bacteria, fungi, or viruses. Thymosin alpha 1 also has anti-inflammatory and anti-fatigue properties and is given to patients with hepatitis B and C, malignant melanoma, liver cancer, drug-resistant tuberculosis, Lyme disease, and DiGeorge’s syndrome (an immunodeficiency disease caused by thymus gland abnormalities). The thymus gland’s production of thymosin alpha 1 highlights its critical role in immune function and therapeutic potential.
How Thymosin Alpha 1 Works
Thymosin alpha 1 stimulates signaling pathways in the immune system. By acting through toll-like receptors (a class of proteins that is essential in the innate immune system), thymosin alpha 1 discourages the replication of viruses, bacteria, fungi, and other harmful microorganisms.
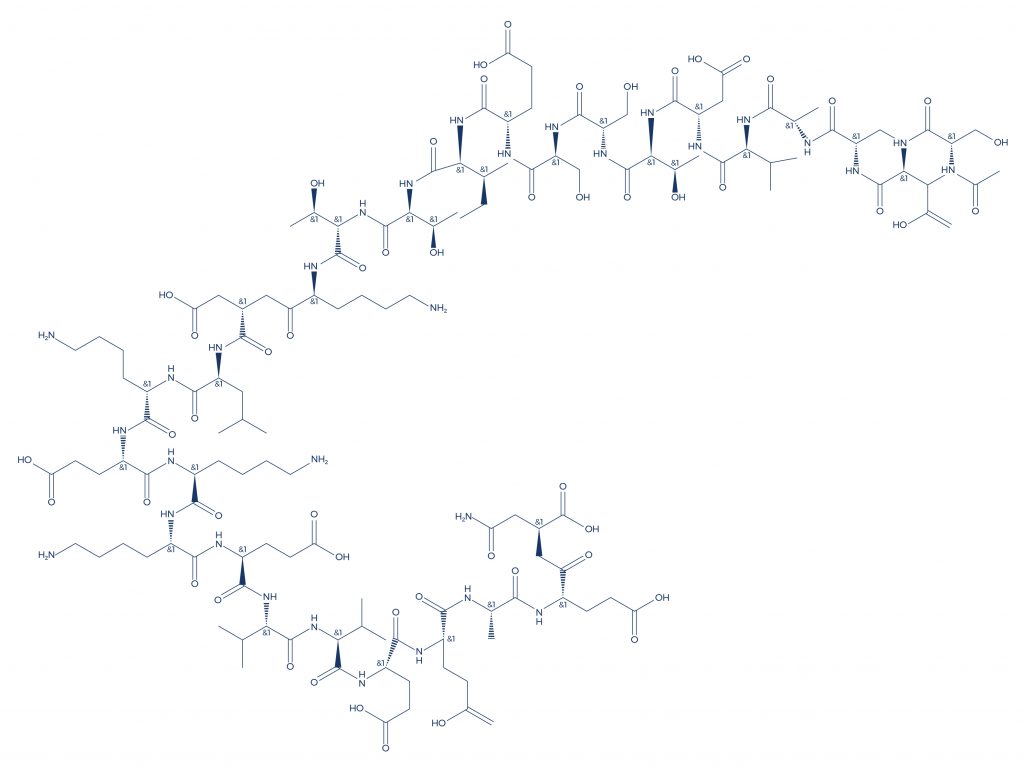
Chemical Structure of Thymosin Alpha 1
Research on Thymosin Alpha 1
A. Eradicates Bacteria, Viruses, and Fungi
Thymosin alpha 1 (Tα1) eradicates bacteria, viruses, and fungi by enhancing the host’s immune response. It stimulates the maturation and activation of T cells, natural killer (NK) cells, and dendritic cells, which are crucial for recognizing and eliminating pathogens. Tα1 also promotes the production of cytokines like interferons and interleukins that boost the innate and adaptive immune systems. Additionally, it helps regulate the balance of pro- and anti-inflammatory responses, reducing immune evasion by pathogens. These combined actions enable Tα1 to combat a wide range of infections effectively while improving overall immune resilience.
- In patients with severe sepsis (the presence of harmful microorganisms in the blood), thymosin alpha 1 administration improved clinical outcomes without any adverse effects, showing potential for broader applications, including conditions like severe acute respiratory syndrome. [1]
- In patients with chronic hepatitis B and C, thymosin alpha 1 administration for 6 months normalized liver enzyme levels, which is suggestive of improved liver function and enhanced cell mediated immune responses. [2]
- In mice with a fungal infection, thymosin alpha 1, a peptide produced by the thymus gland, increased the production of phagocytes, which are cells capable of engulfing and absorbing bacteria. This action highlights the vital role of the thymus gland in immune response, as it supports the production of essential immune cells like phagocytes to combat infections.[3]
- Thymosin alpha 1-based immunomodulatory therapy was associated with a significant reduction in mortality in septic patients, highlighting its potential benefit for individuals with compromised immune systems, such as those affected by acquired immune deficiency syndrome. [4]
- Thymosin alpha 1 administration in septic patients was also associated with increased survival rates, alleviation of illness, and shorter ICU stays and mechanical ventilation times, suggesting potential therapeutic benefits for patients with critical conditions, including those battling lung and breast cancer. [5]
B. Boosts the Function of Certain Immune Cells
Thymosin alpha 1 (Tα1) boosts immune function by enhancing the activity and efficiency of key immune cells, including T lymphocytes, dendritic cells, and natural killer (NK) cells. It promotes T cell differentiation and maturation, particularly aiding cytotoxic T cells in recognizing and attacking infected or malignant cells. Tα1 also enhances the antigen-presenting capacity of dendritic cells, improving immune surveillance. Additionally, it increases the cytotoxic activity of NK cells, helping the immune system target and destroy abnormal cells. By modulating cytokine production and reducing inflammation, Tα1 optimizes the immune response while maintaining balance, making it effective in combating infections, cancer, and immune-related disorders.
- Thymosin alpha 1 is known to augment T-cell function. [6-7]
- Thymosin alpha 1 also helps regulate both the innate and adaptive immune systems. [8-9]
- Thymosin alpha has the ability to increase CD4+/CD8+ ratio. [10-11]
- By activating and stimulating certain signaling pathways, thymosin alpha 1 boosts the production of immune-related cytokines. [12]
- By selectively stimulating the release of luteinizing hormone (LH), thymosin alpha 1 indirectly strengthens the immune function. [13]
- A study found that thymosin alpha 1 can boost the response of the immune system to inactivated vaccines. [14]
- In patients with blood infection (sepsis), thymosin alpha 1 reduced the mortality rate by increasing the production of white blood cells known as monocytes. [15]
- Studies suggest that thymosin alpha 1 can inhibit HIV-1 and human T lymphotropic virus 1 infection by potentiating the release by CD8 (+) cells of soluble factors. [16-17]
C. Suppresses Cancer and Tumor Growth
Thymosin alpha 1 (Tα1) suppresses cancer and tumor growth by enhancing the immune system’s ability to identify and attack malignant cells. It activates cytotoxic T lymphocytes and natural killer (NK) cells, which are critical for targeting and destroying cancer cells. Tα1 also boosts the antigen-presenting function of dendritic cells, improving tumor recognition by the immune system. Additionally, it modulates the production of cytokines such as interferon-γ and interleukins, creating an anti-tumor immune environment. By inhibiting pathways associated with tumor progression, including angiogenesis and inflammation, Tα1 not only strengthens immune defenses but also directly impedes mechanisms that support tumor growth and metastasis.
- By regulating cytokine secretion and repairing the damaged immune system, thymosin alpha 1 may help reduce cancer incidence, offering potential therapeutic benefits for patients with compromised immunity, including those affected by human immunodeficiency virus.[18]
- In the stage IV human breast cancer model, thymosin alpha 1 treatment, which has also been studied for its effects on chronic active hepatitis, was associated with significantly slow tumor growth. [19]
- In patients with metastatic melanoma and advanced non-small cell lung cancer, thymosin alpha 1 treatment prolonged survival. [20]
- In patients with hepatitis B virus-associated liver cancer, thymosin alpha 1 therapy improved liver function and significantly prolonged recurrence‑free and overall survival. [21]
- Thymosin alpha 1 exerts its anti-tumor effects mainly by increasing the secretion of various T cell lymphokines, activating T4 helper cells to promote lymphocyte activity, and increasing the cytotoxicity of natural killer cells. [22-24]
- Administration of thymosin alpha 1 in cancer patients was associated with reduced risk of death and improved disease‐/progression‐free survival. [25]
- In patients with metastatic lung cancer, thymosin alpha 1 treatment was associated with the complete disappearance of lesions. [26]
- A cell study found that exposure of human breast cancer cells to thymosin alpha 1 induced apoptosis (programmed cell death). [27]
- The administration of thymosin alpha 1 in cancer patients increased the anti-tumor effect of chemotherapy while markedly reducing the side effects of the treatment. [28]
- In tumor-bearing mice, thymosin alpha 1 significantly delayed tumor growth and prolonged survival time. [29]
- In mice with breast cancer, thymosin alpha 1 exerted anti-tumor activity by increasing the levels of CD4 and CD8 cells. [30]
- In patients with cancer that had spread to other body parts, thymosin alpha 1 administration increased the survival rate. [31]
- In a human lung cancer cell line, thymosin alpha 1 inhibited cellular proliferation, cell migration, and an increase in the level of damaging free radicals. [32]
- Studies show that thymosin alpha 1 can enhance the anti-cancer effects of chemotherapeutic drugs. [33-34]
D. Accelerates the Wound Healing Process
Thymosin alpha 1 (Tα1) accelerates wound healing by enhancing immune response and promoting tissue repair. It stimulates the activity of immune cells such as macrophages and neutrophils, which clear pathogens and debris from the wound site. Tα1 also boosts fibroblast proliferation and collagen synthesis, essential for rebuilding damaged tissues. By modulating cytokine production, Tα1 creates an anti-inflammatory environment that facilitates healing. Additionally, its ability to enhance angiogenesis, or the formation of new blood vessels, ensures improved oxygen and nutrient delivery to the injured area, further supporting tissue regeneration and recovery.
- In rat kidney cells, thymosin alpha 1 prevented programmed cell death and renal scarring. [3]
- When given either topically or in the form of injections, thymosin alpha 1 accelerated wound healing in mice. [35]
- A cell-based study found that thymosin alpha 1 accelerates wound healing by promoting the formation of new blood vessels and cell migration at the site of injury. [36]
- In neonatal mice, thymosin alpha 1 promoted the formation of new nerve cells or neurons (neurogenesis) by countering lipopolysaccharide-induced impairment. [37]
- In patients with traumatized permanent front teeth, thymosin alpha 1 treatment for 12 months resulted in significant healing of gum tissues. [38]
E. Fights Inflammation
Thymosin alpha-1 peptide combats inflammation by modulating the immune system to restore the balance between pro-inflammatory and anti-inflammatory responses. It reduces excessive inflammation by inhibiting the production of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 while promoting anti-inflammatory cytokines like IL-10. Tα1 also enhances regulatory T cell function, which helps suppress overactive immune responses. Furthermore, it mitigates oxidative stress and prevents the activation of inflammatory pathways such as NF-κB. By fine-tuning the immune response, Tα1 effectively minimizes tissue damage associated with chronic inflammation and supports healing.
- In rats with acute liver failure, thymosin alpha 1 reduced liver inflammation. [39]
- Thymosin alpha 1 may help prevent tissue injury by reducing the release of inflammatory factors and cytokines, and the levels of IL-10 to control inflammation. [40-42]
- Thymosin alpha 1 also reduces inflammation by suppressing pro-inflammatory TNF-α. [43-46]
- A cell-based study also found that thymosin alpha 1 protects against inflammatory allergy. [47]
- In mice with cystic fibrosis, an inherited disease that causes build-up of sticky, thick mucus in the organs and chronic inflammation, thymosin alpha 1 reduced inflammation and associated symptoms. [48]
- In rodents, thymosin alpha 1 reduced the activation of inflammatory responses. [49]
F. Increases Vaccine Effectiveness
Thymosin alpha 1 is the ultimate immune system booster. Studies show that this peptide can naturally enhance the effectiveness of certain vaccines:
- In patients who are susceptible to infection, thymosin alpha 1 administration enhanced the immunogenicity (ability to provoke an immune response) of the pandemic influenza vaccine. [50]
- In elderly patients, administration of thymosin alpha 1 together with influenza vaccine enhanced vaccine responses. [51-52]
- In animal models, thymosin alpha 1 enhanced the efficacy of the classical swine fever vaccine. [53]
Thymosin Alpha 1 Side Effects
Thymosin alpha 1 side effects are very uncommon. There have been some side effects associated with the use of this drug wherein the patient had one of the issues listed below at some point while being on thymosin alpha 1. However, these side effects weren’t confirmed to be associated with the treatment and could have been a coincidence and not related to the use of thymosin alpha 1. Despite this, it was listed as a side effect associated with thymosin alpha 1 even though these associated side effects are very uncommon.
Side effects associated with thymosin alpha 1 may include the following:
- Fatigue
- Fever
- Low white blood cells
- Muscle aches
- Nausea
- Vomiting
Thymosin Alpha 1 Dose
Thymosin Alpha 1 (Tα1) is a synthetic version of a naturally occurring peptide produced by the thymus gland, widely used for its immune-modulating properties, particularly in the context of virally infected cells. Its dosing largely depends on the condition being treated, patient-specific factors such as age, weight, and overall health, and the desired therapeutic outcome. The most common method of administration is subcutaneous injection, allowing the drug to be absorbed into the bloodstream gradually. Clinical research and medical guidelines provide standardized dose ranges for various applications, but individual adjustments may be necessary under the supervision of a healthcare provider.
For chronic infections like hepatitis B or C, the typical dose of Thymosin Alpha 1 ranges from 1.6 mg to 3.2 mg administered twice weekly for a duration of six months or longer, depending on the patient’s response. In cancer immunotherapy, particularly in combination with other treatments, dosages may vary between 1.6 mg to 6.4 mg per week, often tailored to complement the overall therapeutic regimen. For acute conditions like sepsis or severe respiratory infections, higher doses administered over shorter periods may be employed to enhance rapid immune activation, particularly by stimulating immune reconstitution.
The dosing of Thymosin Alpha 1 must be carefully adjusted for patients with compromised organ function, such as those with advanced liver disease or chronic kidney conditions. Additionally, immunocompromised individuals or elderly patients may require tailored dosing strategies to achieve optimal efficacy while minimizing potential side effects. Clinical trials have demonstrated the safety of Thymosin Alpha 1 even at higher doses, but long-term safety data continue to guide its use. Patients are advised to consult their healthcare providers for personalized dosing plans that align with their medical history and treatment objectives.
Thymosin Alpha 1 How Long to Take
The length of time a patient should take Thymosin Alpha 1 (Tα1) depends on the specific condition being treated and the therapeutic goals. For chronic infections like hepatitis B or C, treatment durations often span six months or longer. This extended timeframe allows sufficient time for immune modulation and liver enzyme normalization, which are critical for achieving lasting benefits. In cancer research, studies involving human cancer cell lines have provided insights into the potential role of Tα1 in immune modulation, influencing its therapeutic applications. In some cases, treatment may be continued beyond six months, depending on the patient’s response and the advice of a healthcare provider.
In acute situations, such as sepsis or severe viral infections, Thymosin Alpha 1 is typically administered over shorter periods, ranging from a few days to a few weeks. The aim in these cases is to provide rapid immune support, reduce inflammation, and stabilize the patient’s condition, thereby reducing the risk of complications such as multiple organ failure. Once the acute phase has resolved and the patient shows significant improvement, the treatment may be discontinued. However, follow-up monitoring is essential to ensure no relapse or lingering immune dysfunction.
For patients with chronic diseases, immune deficiencies, or as part of cancer immunotherapy, Thymosin Alpha 1 may be used as a long-term or maintenance therapy. In such cases, treatment may be administered in cycles, such as weekly injections over several months, followed by periods of observation. This cyclic approach helps sustain immune function while minimizing the risk of side effects or immune tolerance. The decision to continue or stop treatment is highly individualized, based on regular assessments of the patient’s health, treatment efficacy, and overall goals of care.
Thymosin alpha 1 Injection
Thymosin Alpha 1 (Tα1) injection is a peptide-based therapy widely recognized for its immunomodulatory properties. Administered via subcutaneous injection, Tα1 works by stimulating the production and activity of T-cells, enhancing the immune system’s ability to fight infections, cancer, and other diseases. It also plays a critical role in regulating immune and inflammatory responses, making it particularly beneficial for individuals with compromised immune systems, such as those suffering from chronic viral infections like hepatitis B and C, autoimmune disorders, or undergoing chemotherapy. The injection form ensures efficient delivery and rapid absorption into the bloodstream, maximizing its therapeutic potential.
Thymosin Alpha 1 injections have demonstrated efficacy across a range of medical conditions. In clinical settings, they are used to reduce disease severity in sepsis, support recovery from viral infections, and enhance vaccine responses, particularly in immunocompromised patients. Additionally, Tα1 has shown promise as an adjunctive treatment in cancer immunotherapy by boosting tumor antigen recognition and improving immune-mediated tumor suppression. Research indicates that regular administration of Tα1 injections can lead to improved survival rates, reduced inflammation, and better overall clinical outcomes in patients with severe immune dysfunctions.
The dosage and frequency of Thymosin Alpha 1 injections depend on the patient’s condition and the desired therapeutic outcomes. Commonly, doses range from 0.9 mg to 1.6 mg administered twice weekly for several weeks to months, as recommended by a healthcare provider. The subcutaneous injection is typically given in the upper arm, thigh, or abdomen, and is well-tolerated with minimal side effects. Patients should follow their prescribed regimen closely and consult with their physician to adjust the dosage if needed, based on their response to treatment and overall health status. Proper administration and adherence to the injection schedule are crucial for achieving optimal benefits.
Is Thymosin Alpha 1 10mg Good?
Thymosin Alpha 1 (Tα1) is a peptide known for its ability to modulate immune responses and enhance the body’s defense against infections and malignancies. A 10mg dose of Thymosin Alpha 1 is typically presented as a vial containing the active ingredient, which is then diluted and administered in smaller subcutaneous doses based on the patient’s treatment plan. This dosage provides flexibility for tailoring treatment regimens to individual needs, allowing for precise adjustments in therapy to manage conditions such as chronic viral infections, autoimmune diseases, and immune deficiencies.
The 10mg formulation of Thymosin Alpha 1 is not administered all at once; rather, it is divided into multiple doses over several weeks or months. This approach ensures sustained therapeutic effects while minimizing the risk of side effects. Clinical studies have shown that Tα1 at recommended doses significantly enhances immune function, promotes T-cell activity, and supports the resolution of inflammation. Patients with chronic conditions like hepatitis B, certain cancers, and autoimmune disorders often experience notable improvements in immune markers and clinical symptoms when treated with Tα1. Thus, the 10mg vial serves as a convenient and effective starting point for various treatment protocols.
The appropriateness of using a 10mg vial of Thymosin Alpha 1 depends on the individual’s medical condition, the severity of their immune dysfunction, and their specific therapeutic goals. Healthcare providers assess these factors before determining the dosage and frequency of administration. Thymosin Alpha 1 is thought to exert its effects partly by acting on T cell progenitor cells, supporting the development and activation of the immune system. Importantly, Tα1 is known for its excellent safety profile, with minimal side effects reported even in long-term use. However, as with any treatment, adherence to a prescribed regimen and close monitoring by a physician are essential to achieve optimal results. For many patients, the 10mg formulation offers a practical and effective way to harness the benefits of Thymosin Alpha 1 for improved health outcomes.
Thymosin Alpha 1 Cancer
Thymosin Alpha 1 (Tα1) has emerged as a promising immunomodulatory agent in cancer therapy due to its ability to enhance the immune system’s ability to fight tumors. It works by stimulating T cells and natural killer (NK) cells, which play a critical role in detecting and destroying cancer cells. Additionally, Tα1 upregulates the expression of major histocompatibility complex (MHC) class I molecules on tumor cells, improving their visibility to the immune system. This dual action of boosting immune response and increasing tumor cell recognition positions Tα1 as a valuable adjunct in cancer treatment strategies, particularly in combination with chemotherapy, radiation, or immune checkpoint inhibitors.
Studies and clinical trials have demonstrated the efficacy of Tα1 in several types of cancers, including melanoma, non-small cell lung cancer, and hepatocellular carcinoma. For instance, combining Tα1 with standard chemotherapy has been shown to improve overall survival rates and reduce treatment-related side effects. Its ability to modulate cytokine production and reduce inflammation also contributes to an improved tumor microenvironment, which can hinder cancer progression. Additionally, Tα1 has been observed to inhibit viral replication in cancer patients who may have coexisting viral infections, further enhancing its therapeutic value. Notably, in patients with compromised immunity due to cancer or its treatment, Tα1 helps restore immune function and may also indirectly suppress viral replication, enabling the body to better cope with the disease and associated therapies.
One of the significant advantages of Thymosin Alpha 1 in cancer therapy is its excellent safety profile. Unlike many conventional cancer treatments, Tα1 has minimal side effects, making it suitable for prolonged use alongside other therapies. Its ability to support the immune system is particularly beneficial for patients with advanced-stage cancers or those undergoing aggressive treatment regimens. While more extensive studies are needed to establish its full potential across various cancer types, existing evidence suggests that Tα1 could become a cornerstone in integrative cancer care, offering hope for improved outcomes and enhanced quality of life for patients battling this challenging disease.
Thymosin Alpha 1 Autoimmune Disease
Thymosin Alpha 1 (Tα1) has shown significant potential in managing autoimmune diseases by modulating the immune system to restore balance. Autoimmune diseases occur when the immune system mistakenly attacks healthy cells, often leading to chronic inflammation and tissue damage. Tα1 helps address this imbalance by promoting regulatory T cell (Treg) activity, which plays a crucial role in suppressing overactive immune responses. Furthermore, Tα1 can enhance cell-mediated immunity, supporting the body’s ability to fight infections while maintaining immune regulation. Additionally, it modulates cytokine production, reducing pro-inflammatory markers such as TNF-α and IL-6 while enhancing anti-inflammatory pathways, making it an attractive option for conditions like multiple sclerosis, rheumatoid arthritis, and lupus.
The immunomodulatory properties of Tα1 are central to its role in autoimmune disease therapy. By enhancing the function of dendritic cells and natural killer cells, Tα1 not only reduces excessive immune activation but also supports the maintenance of immune tolerance. This dual mechanism allows it to mitigate autoimmune attacks while still preserving the immune system’s ability to combat infections and other threats. Furthermore, Tα1 promotes the regeneration of damaged tissues by supporting cellular repair processes, which is particularly beneficial in diseases characterized by chronic inflammation and tissue destruction.
Tα1 has been evaluated in various clinical trials and experimental settings for its efficacy in autoimmune diseases, often showing promising results in reducing disease severity and progression. One of the key advantages of Tα1 is its favorable safety profile, as it is generally well-tolerated and has minimal side effects compared to traditional immunosuppressive drugs. This makes it a valuable therapeutic option, particularly for patients who experience severe side effects from existing treatments or those requiring long-term management. While further research is needed to fully elucidate its long-term efficacy across different autoimmune conditions, Tα1 holds significant promise as a safe and effective addition to autoimmune disease treatment protocols.
Thymosin Alpha 1 Supplement
Thymosin Alpha 1 (Tα1) supplements are designed to harness the immunomodulatory properties of this naturally occurring peptide, which is derived from the thymus gland. As a supplement, Tα1 supports the immune system by enhancing the function of T cells, promoting cytokine production, and regulating inflammatory responses. These attributes make Tα1 supplements attractive for individuals seeking to boost immunity, especially in the context of chronic infections, weakened immune function, or as a complementary approach to existing therapies. For individuals on highly active antiretroviral therapy, Tα1 may provide additional support by improving immune function and helping the body better manage the effects of chronic viral infections.
Tα1 supplements have been studied for their potential in managing a wide range of health conditions, including autoimmune diseases, viral infections, and even as adjunctive therapy in cancer treatment. By improving the body’s immune response, Tα1 supplements may help reduce the risk of infections and support recovery in conditions where immune dysfunction is a concern. Additionally, their anti-inflammatory properties may provide benefits in managing chronic inflammation, a common underlying factor in many health disorders. These supplements are often considered as part of integrative approaches to enhance overall health and resilience.
While Tα1 supplements are generally regarded as safe, their use should be guided by healthcare professionals to ensure proper dosage and monitoring. They are typically well-tolerated, with minimal side effects compared to more aggressive pharmaceutical interventions. However, as with any supplement, individuals should consider potential interactions with other medications and underlying health conditions. Further research is ongoing to establish the full scope of Tα1’s efficacy and optimal use, but preliminary studies suggest promising results for its role in supporting immune health, reducing inflammation, and enhancing cell-mediated immunity, particularly in individuals with compromised immune systems or chronic infections.
Thymosin Alpha 1 vs Thymosin Beta 4
Thymosin Alpha 1 (Tα1) and Thymosin Beta 4 (Tβ4) are peptides derived from the thymus gland, each playing distinct roles in regulating immune functions and tissue repair. Tα1 primarily acts as an immunomodulator, enhancing T-cell activity, promoting cytokine production, and regulating immune responses. It is commonly used in managing chronic infections, and autoimmune diseases, and as an adjunct therapy in cancer treatment due to its recognized immune-modulating capacity. On the other hand, Tβ4 is known for its role in tissue repair and regeneration, promoting angiogenesis, reducing inflammation, and aiding wound healing by facilitating cell migration and proliferation.
The primary difference between Tα1 and Tβ4 lies in their mechanisms of action and therapeutic targets. Tα1 focuses on modulating immune responses, making it valuable in conditions involving immune deficiencies, such as chronic viral infections or weakened immune function. Conversely, Tβ4 is more associated with physical recovery and regeneration, commonly used in scenarios like sports injuries, surgical wound healing, and cardiovascular repair. While Tα1 is noted for its ability to boost immune defense, Tβ4 is widely regarded for its cytoprotective properties and its ability to promote rapid tissue recovery. Notably, Tα1 has shown promise in supporting treatments for cancers such as renal cell carcinoma, enhancing immune response to improve patient outcomes.
Despite their differences, Tα1 and Tβ4 can have complementary roles in therapy. For instance, in conditions involving both immune dysfunction and tissue damage, such as certain autoimmune diseases or post-surgical recovery, the combined use of these peptides may address multiple aspects of healing and resilience. Tα1 is particularly notable for its ability to kill virally infected cells, enhancing the body’s immune response against chronic or acute infections. However, their administration should be guided by clinical evaluation to ensure that the specific needs of the patient are met. While both peptides show promising therapeutic potential, further research is essential to optimize their use and to explore how they might synergistically enhance treatment outcomes in complex conditions.
Thymulin vs Thymosin Alpha 1
Thymulin and Thymosin Alpha 1 (Tα1) are thymus-derived peptides with distinct roles in immune regulation. Thymulin primarily acts as a neuroendocrine modulator and an immune regulator, influencing T-cell differentiation and modulating the activity of various cytokines. It is particularly known for its role in enhancing the functional activity of natural killer (NK) cells and cytotoxic T lymphocytes. In contrast, Tα1 is a powerful immunomodulator with broader effects, including boosting T-cell activity, promoting cytokine production, and improving the immune system’s response to infections and cancers. Notably, Tα1 also kills virally infected cells, strengthening the body’s ability to combat chronic and acute viral infections. Both peptides are associated with improving immune resilience, but they operate through different mechanisms and are used for distinct therapeutic applications.
The primary distinction between thymulin and Tα1 lies in their functional targets and therapeutic potential. Thymulin has been widely studied for its neuroimmunomodulatory properties and its role in balancing the immune system in autoimmune and inflammatory conditions. It is also linked to the regulation of circadian rhythms and hormonal responses. Meanwhile, Tα1 is recognized for its ability to enhance the immune system’s capacity to combat chronic infections, autoimmune diseases, and cancers. Tα1 has gained FDA approval for certain conditions, such as hepatitis B and C, and is frequently used as an adjunct therapy in cancer immunotherapy. Importantly, Tα1 can also help address chemotherapy induced immune depression, supporting patients’ immune recovery during and after treatment. Thymulin, while promising, is still under investigation for clinical use in similar capacities.
Although thymulin and Tα1 have different primary actions, they can be complementary in managing complex immune-related conditions. For instance, thymulin’s ability to modulate immune balance and reduce inflammation might synergize with Tα1’s immune-boosting effects in conditions like autoimmune diseases or chronic infections. Additionally, thymulin’s influence on neuroendocrine-immune interactions may support overall homeostasis, enhancing the therapeutic outcomes of Tα1. Research into their combined use is limited but holds promise for developing more effective treatments targeting both immune regulation and systemic resilience.
Thymosin Alpha 1 Nasal Spray
Thymosin Alpha 1 (Tα1) is a peptide with significant immunomodulatory properties, typically administered through injections. However, the nasal spray formulation offers a non-invasive alternative that directly targets the mucosal immune system. The nasal route allows Tα1 to interact with the immune cells in the nasal and respiratory mucosa, stimulating localized and systemic immune responses. This method is particularly promising for respiratory infections, autoimmune diseases, and conditions requiring rapid immune activation, as the nasal mucosa serves as a frontline barrier against pathogens. Furthermore, Tα1’s effects include promoting B cell growth factors, which support the development and function of B cells crucial for humoral immunity.
The nasal spray delivery of Tα1 presents several advantages over traditional injection-based methods. It is less invasive, improving patient compliance, especially for those requiring long-term therapy. The direct application to the nasal mucosa can lead to faster onset of immune activation, particularly beneficial for respiratory illnesses or acute infections. Furthermore, nasal administration bypasses the first-pass metabolism in the liver, potentially enhancing the bioavailability of Tα1. This method is being explored for its effectiveness in treating chronic conditions like asthma, allergies, and even viral infections where mucosal immunity plays a critical role. Notably, Tα1 can target respective target infected cells, enhancing the immune system’s ability to neutralize pathogens at their initial site of entry.
Although the nasal spray formulation of Tα1 is still under investigation, early studies and clinical trials show promise in expanding its therapeutic applications. Researchers are exploring its efficacy in treating upper respiratory tract infections, chronic rhinosinusitis, and as an adjunct therapy for viral illnesses such as influenza and COVID-19. Additionally, the nasal delivery system may offer opportunities for combination therapies, where Tα1 can be paired with other immune-enhancing agents for synergistic effects. As research progresses, Tα1 nasal spray could become a widely used immunotherapy, offering an effective and user-friendly approach to enhancing immune health.
Thymosin Alpha 1 for Injection 1.6 mg
Thymosin Alpha 1 (Tα1) for injection at a dose of 1.6 mg is a purified synthetic version of a naturally occurring peptide produced by the thymus gland. It is widely recognized for its immunomodulatory properties, making it beneficial in treating conditions associated with immune dysfunction. The 1.6 mg dosage is often used in clinical settings to boost the immune response in patients with chronic infections, cancer, and autoimmune diseases. Its ability to enhance T-cell function and regulate cytokine production has made it a valuable adjunct therapy for immune-related conditions. Additionally, Tα1 shows potential in inhibiting tumor cell proliferation, contributing to its role in cancer treatment strategies.
The 1.6 mg dose of Tα1 is commonly administered to support the immune system in patients with viral infections such as hepatitis B, hepatitis C, and even certain respiratory conditions. It is also employed as part of cancer immunotherapy regimens to enhance the efficacy of chemotherapy and radiation by improving the body’s natural defenses. Additionally, Tα1 at this dosage is effective in addressing sepsis and other critical illnesses where immune suppression is a concern. Its relatively small yet potent dose ensures therapeutic efficacy while minimizing the risk of side effects.
Thymosin Alpha 1 for injection is administered subcutaneously, ensuring direct entry into the systemic circulation for optimal immune modulation. The 1.6 mg dose is typically given once or twice weekly, depending on the patient’s condition and therapeutic goals. Clinical studies and patient data suggest that this dosage is well-tolerated, with minimal side effects, such as mild injection site reactions. The safety profile of Tα1 has been extensively studied, and it is generally regarded as safe for use across diverse patient populations. This dosage continues to be a cornerstone in immunotherapy protocols, offering a targeted approach to restoring immune balance.
FAQ
What is the function of thymosin alpha 1?
Thymosin Alpha 1 functions as an immunomodulatory peptide that enhances T-cell activity, regulates cytokine production, and strengthens the immune system’s ability to combat infections, cancer, and immune-related disorders. Its effects on immune function are partly mediated through the regulation of cell receptor excision circles, which play a key role in T-cell development and immune responses. Additionally, research has shown that thymosin alpha 1 influences cell receptor excision circles, helping to improve the efficacy of immune responses and offering potential therapeutic benefits. By modulating these cell receptor excision circles, Thymosin Alpha 1 enhances immune system function in various clinical contexts.
What are the side effects of thymosin alpha 1?
Thymosin alpha 1 is generally well-tolerated, with rare side effects including mild redness or irritation at the injection site. In patients with chronic hepatitis C, thymosin alpha 1 has shown potential benefits in improving immune function. Additionally, its use in individuals with chronic hepatitis C may help enhance the response to antiviral treatments.
What does thymosin do to the body?
Thymosin enhances immune function by promoting T-cell activity, regulating inflammation, and supporting immune system balance. This can be particularly beneficial for individuals with chronic hepatitis C, as the peptide may help boost immune responses to manage the virus. Additionally, thymosin’s ability to regulate inflammation could offer potential support for those suffering from chronic hepatitis C, as persistent inflammation is a key issue in the progression of the disease.
What are the benefits of thymosin peptide?
Thymosin peptides boost immunity, reduce inflammation, enhance infection and cancer resistance, and support tissue repair and regeneration by stimulating the adaptive immune response. These peptides play a crucial role in modulating the adaptive immune response, promoting the activation of immune cells that are key in defending against infections and cancers. Additionally, thymosin peptides contribute to tissue healing by fostering an effective adaptive immune response, which aids in repair and regeneration processes.
What is thymosin and what does it do?
Thymosin refers to a group of peptides, including thymosin alpha 1, which regulate immune responses and support cell-mediated immunity. These peptides play a crucial role in t cell maturation, enhancing the development and activation of T cells. By supporting t cell maturation, thymosin contributes to the regulation of immune responses. Additionally, its role in promoting t cell maturation is vital for maintaining a balanced and effective immune system.
Is thymosin a steroid or protein?
Thymosin is a peptide, which is a type of protein fragment. Research has identified its potential in supporting immune function and reducing complications associated with critical conditions like multiple organ failure. Thymosin’s role in modulating immune responses is particularly significant in preventing or managing multiple organ failure in severe infections or trauma. Ongoing studies continue to explore its therapeutic applications in various conditions, including those involving multiple organ failure.
What is TA1 for?
TA1 (Thymosin Alpha 1), often derived through genetic engineering production, is used to enhance immune function, treat immune deficiencies, and support therapies for infections, cancer, and autoimmune diseases. The genetic engineering production process ensures high purity and efficacy of TA1 for medical applications. This peptide’s ability to modulate the immune system effectively makes it a valuable product of genetic engineering production in modern medicine.
How long to take thymosin alpha 1?
The duration of thymosin alpha 1 therapy varies depending on the condition, typically ranging from several weeks to months under medical supervision. Research into thymosin alpha 1 has often involved the use of stable cell lines to evaluate its mechanisms and efficacy. These stable cell lines provide a controlled environment for understanding its therapeutic potential. Additionally, stable cell lines are crucial for the consistent production and testing of thymosin alpha 1 in various medical applications.
Is thymosin a peptide or steroid?
Thymosin is a peptide, with no significant adverse effects observed in most studies. It is used in various medical and therapeutic applications, and significant adverse effects observed have been minimal in clinical trials. Overall, thymosin demonstrates a favorable safety profile, with significant adverse effects observed being rare and generally mild.
What is the primary function of thymosin?
The primary function of thymosin is to modulate the immune system, primarily by activating T-cells and enhancing immune defense mechanisms. Thymosin also plays a crucial role in regulating immune and inflammatory responses, ensuring the body can effectively respond to infections and injuries. Additionally, its ability to influence immune and inflammatory responses highlights its importance in maintaining overall immune system balance. Emerging research suggests thymosin may also have therapeutic applications in disorders involving dysregulated immune and inflammatory responses.
How long does thymosin alpha 1 last?
Thymosin alpha 1 has a half-life of approximately 2 hours, with effects depending on the dosing regimen and condition being treated. This peptide is often explored as part of a combination therapy to enhance its effectiveness in various medical conditions. Researchers are investigating how thymosin alpha 1 can be integrated into combination therapy approaches to maximize therapeutic outcomes. The potential benefits of thymosin alpha 1 in combination therapy highlight its versatility in addressing complex health issues.
What happens if you have too little thymosin?
A deficiency in thymosin can lead to weakened immune function, making the body more susceptible to infections and diseases. Studies have shown that thymosin and interferon alpha may play complementary roles in modulating the immune response. When thymosin levels are deficient, the body’s ability to work in synergy with interferon alpha may also be compromised, further impacting immune defense. Understanding the relationship between thymosin and interferon alpha is critical for developing therapies to boost immune function.
What is thymosin alpha 1 injection used for?
Thymosin alpha 1 injection, produced using a yeast expression system, is used to enhance immune function, treat infections, and support therapies for cancer and autoimmune diseases. The yeast expression system allows for efficient and scalable production of this peptide, ensuring high purity and efficacy. This system has been identified as a reliable method for producing Thymosin alpha 1 for medical applications.
What are the effects of thymosin alpha 1?
Thymosin alpha 1 boosts immune system activity, regulates inflammation, and enhances T-cell responses to infections and tumors. Recent advances in genetic engineering expression have facilitated the production of thymosin alpha 1 for research and therapeutic purposes. These developments in genetic engineering expression have improved its availability and consistency for clinical applications. Additionally, ongoing studies using genetic engineering expression aim to optimize its efficacy in treating immune-related conditions.
What are the benefits of thymosin injections?
Thymosin injections improve immune health, reduce inflammation, support cancer therapy, and enhance recovery from infections and immune-related conditions. Additionally, thymosin has been linked to increased cell growth factor production, which plays a key role in tissue repair and immune system function. The cell growth factor production promoted by thymosin injections further contributes to the body’s ability to recover and regenerate. This process also supports overall immune health by boosting cell growth factor production, aiding in the healing of damaged tissues.
What effect does thymosin have on the body?
Thymosin enhances immune regulation, improves T-cell function, and promotes the body’s ability to fight infections and diseases. By restoring immune function, Thymosin helps strengthen the body’s defense mechanisms. Additionally, its ability to stimulate immune responses plays a crucial role in restoring immune function, ensuring more effective protection against pathogens.
Where to inject thymosin alpha 1?
Thymosin alpha 1 is typically injected subcutaneously into fatty tissue, such as the abdomen or thigh. It has been studied for its potential benefits in patients with advanced HIV disease, where it may help modulate the immune response. Additionally, Thymosin alpha 1 has shown promise in improving immune function in individuals with advanced HIV disease, potentially supporting the body in combating infections and managing symptoms associated with the condition.
What is TA1 for cancer patients?
TA1 (Thymosin Alpha 1) helps enhance the immune response, improves cancer treatment outcomes, and reduces infection risks in cancer patients. Studies have shown that TA1 may also have an effect on human breast cancer lines, improving the efficacy of treatment. Additionally, research on human breast cancer lines suggests that TA1 could potentially inhibit tumor growth and support immune system function in cancer therapies.
What is thymosin beta 4 for cancer patients?
Thymosin beta 4 may aid tissue repair and reduce inflammation in cancer patients but is less directly involved in immune modulation than thymosin alpha 1. While it plays a role in tissue healing, thymosin beta 4’s impact on immune response is less pronounced in comparison to its influence on other factors like tissue regeneration, making it less relevant for treating infectious diseases. However, its potential applications in reducing inflammation could still be useful in managing complications arising from infectious diseases.
When to take thymosin alpha 1?
Thymosin alpha 1 is taken as prescribed, often administered a few times weekly, depending on the condition being treated. Research suggests that Thymosin alpha 1 may have a role in regulating liver superoxide dismutase levels, which helps reduce oxidative stress. The peptide has been identified as a potential modulator of liver superoxide dismutase, contributing to liver health and overall antioxidant defense. Additionally, its effects on liver superoxide dismutase could play a role in improving immune function and reducing inflammation.
How to naturally heal autoimmune disease?
Autoimmune diseases may benefit from a healthy diet, regular exercise, stress management, and supplements like omega-3 fatty acids and vitamin D to reduce inflammation. Additionally, research has shown that immature cord blood lymphocytes can play a role in modulating immune responses, which could be important in managing autoimmune conditions. Supplements that promote immune balance may support the function of immature cord blood lymphocytes, potentially aiding in immune system regulation.
What is the rarest autoimmune disorder?
The rarest autoimmune disorder is likely Goodpasture syndrome, which affects the lungs and kidneys. Researchers have explored various techniques for studying such disorders, including solid phase synthesis, a method used to develop therapeutic peptides. Solid phase synthesis has proven valuable in the creation of compounds that could potentially help manage autoimmune diseases like Goodpasture syndrome.
What is the best anti-inflammatory for autoimmune disease?
The best anti-inflammatory for autoimmune disease depends on the condition, but corticosteroids and biologics like TNF inhibitors are commonly used. In some cases, immune deficiency treatment may also involve the use of immunosuppressive drugs to control inflammation. For individuals with specific autoimmune conditions, immune deficiency treatment tailored to reduce overactive immune responses can help improve quality of life and manage symptoms.
What is thymosin alpha 1 good for?
Thymosin alpha 1 is good for boosting immune function, reducing inflammation, and supporting treatment for infections, cancer, and autoimmune diseases.
What are the side effects of Thymogen Alpha 1?
Thymogen Alpha 1 may cause mild side effects like redness or swelling at the injection site and rarely, fatigue or headache.
What is another name for thymosin alpha 1?
Thymosin alpha 1 is also known as TA1 or Zadaxin.
What does thymosin beta 4 do to the body?
Thymosin beta 4 promotes tissue repair, reduces inflammation, and enhances cellular regeneration and wound healing.
What is the function of thymosin alpha-1?
Thymosin alpha-1 boosts immune system function, activates T-cells, and regulates inflammation.
Is TB 500 thymosin beta 4?
TB 500 is a synthetic version of thymosin beta 4 designed for therapeutic use.
Does thymosin beta 4 build muscle?
Thymosin beta 4 indirectly supports muscle growth by promoting tissue repair and reducing inflammation.
Is thymulin the same as thymosin?
Thymulin and thymosin are different; thymulin regulates T-cell activity, while thymosin is a broader term for thymic peptides like thymosin alpha 1.
What does thymulin peptide do?
Thymulin peptide modulates immune function by enhancing T-cell activity and regulating inflammation.
What is thymalin used for?
Thymalin is used to improve immune function, support recovery from infections, and manage age-related immune decline.
What is thymosin alpha 1 for autoimmune disease?
Thymosin alpha 1 helps regulate the immune system and reduce inflammation, making it effective in treating autoimmune diseases.
What is thymosin alpha 1 for injection 1.6 mg used for?
Thymosin alpha 1 injection 1.6 mg is used to boost immunity and treat infections, cancer, and immune-related disorders.
Reference
Wu J, Zhou L, Liu J, et al. The efficacy of thymosin alpha 1 for severe sepsis (ETASS): a multicenter, single-blind, randomized and controlled trial. Crit Care. 2013;17(1):R8. Published 2013 Jan 17. doi:10.1186/cc11932.
- The efficacy of thymosin alpha 1 for severe sepsis (ETASS): a multicenter, single-blind, randomized and controlled trialA multicenter randomized trial investigated the effects of thymosin alpha 1 (Tα1) on severe sepsis, revealing that Tα1 therapy may improve 28-day survival rates and immune function. Among 361 patients, the Tα1 group showed a reduced mortality rate (26.0% vs. 35.0% in the control group) and significant improvements in immune markers like monocyte HLA-DR levels on days 3 and 7. These findings suggest Tα1, when combined with standard care, could enhance outcomes in severe sepsis without causing serious adverse effects, warranting further research into its immunomodulatory benefits.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4056079/.
Ancell CD, Phipps J, Young L. Thymosin alpha-1. Am J Health Syst Pharm. 2001;58(10):879-85.
- Thymosin alpha-1Thymosin alpha-1 (TA1) is a synthetic polypeptide under investigation for its immune-modulating properties, particularly in hepatitis B and C. TA1 enhances T-cell function and is quickly absorbed with a serum half-life of two hours. Clinical trials for hepatitis B showed mixed results, with HBV DNA clearance rates ranging from 40.6% to 53% in treated patients, compared to lower rates in controls. For hepatitis C, TA1 combined with interferon alfa-2b improved outcomes, with higher rates of ALT normalization and viral RNA clearance than interferon alone. TA1 is well-tolerated, causing minimal side effects like injection site irritation, and is administered subcutaneously twice weekly. While promising, further studies are needed to assess its impact on long-term outcomes.You can read the abstract of the article at https://academic.oup.com/ajhp/article-abstract/58/10/879/5149632.
Romani L, Bistoni F, Gaziano R, et al. Thymosin alpha 1 activates dendritic cells for antifungal Th1 resistance through toll-like receptor signaling. Blood. 2004;103(11):4232-9.
- Thymosin alpha 1 activates dendritic cells for antifungal Th1 resistance through toll-like receptor signalingThymosin alpha 1 enhances antifungal immunity by promoting the maturation and interleukin-12 production of Aspergillus fumigatus-pulsed dendritic cells via the p38 MAPK/NF-kB pathway and Toll-like receptor signaling. In vivo, it activates Th1-dependent immune responses, accelerates myeloid recovery, and protects immunocompromised mice from aspergillosis. This highlights its potential as a therapeutic adjuvant for coordinating innate and adaptive antifungal immunity.You can read the full article at https://www.sciencedirect.com/science/article/pii/S0006497120554207?via%3Dihub.
Li C, Bo L, Liu Q, Jin F. Thymosin alpha1 based immunomodulatory therapy for sepsis: a systematic review and meta-analysis. Int J Infect Dis. 2015;33:90-6.
- Thymosin alpha1 based immunomodulatory therapy for sepsis: a systematic review and meta-analysisA systematic review and meta-analysis of 12 clinical trials involving 1,480 patients found that thymosin alpha 1 (Tα1) immunomodulatory therapy significantly reduced all-cause mortality in septic patients (risk ratio 0.68, 95% CI 0.59–0.78, p<0.00001). While promising, the findings should be interpreted cautiously due to the small sample sizes and variable quality of the included studies, highlighting the need for larger, well-designed multicenter trials to confirm its clinical utility.You can read the full article at https://www.ijidonline.com/article/S1201-9712(14)01750-0/fulltext.
Feng Yun Wang, Bin Fang, XinHuaQiang, et al., “The Efficacy and Immunomodulatory Effects of Ulinastatin and Thymosin α1 for Sepsis: A Systematic Review and Meta-Analysis,” BioMed Research International, vol. 2016, Article ID 9508493, 8 pages, 2016. https://doi.org/10.1155/2016/9508493.
- The Efficacy and Immunomodulatory Effects of Ulinastatin and Thymosin α1 for Sepsis: A Systematic Review and Meta-AnalysisA meta-analysis of six randomized controlled trials involving 944 septic patients found that combined ulinastatin and thymosin α1 (UTI) therapy significantly improved the 28-day survival rate (OR 2.01, 95% CI [1.53, 2.64]) and reduced illness severity as reflected by lower APACHE II scores. UTI treatment also shortened ICU stays and mechanical ventilation times and increased CD4+ T cell levels, suggesting potential immunomodulatory benefits. These findings support UTI as a promising therapy for sepsis, though further research is needed to confirm these outcomes.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4906180/.
Serrate SA, Schulof RS, Leondaridis L, Goldstein AL, Sztein MB. Modulation of human natural killer cell cytotoxic activity, lymphokine production, and interleukin 2 receptor expression by thymic hormones. J Immunol. 1987;17:2338–2343.
- Modulation of human natural killer cell cytotoxic activity, lymphokine production, and interleukin 2 receptor expression by thymic hormonesThymosin fraction 5 (TF5) enhances natural killer (NK) cell activity in vitro by stimulating human large granular lymphocytes (LGL), with additive effects observed when combined with recombinant interferon-alpha. TF5 also promotes interleukin-2 production, interleukin-2 receptor expression, and interferon-gamma production in mitogen-stimulated LGL. Thymosin-alpha 1, derived from TF5, similarly enhances LGL functions, suggesting it is the active component. These findings indicate thymic hormones may regulate NK activity by inducing lymphokine production and receptor expression.You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/3116079/.
Sztein MB, Serrate SA. Characterization of the immunoregulatory properties of thymosin alpha 1 on interleukin-2 production and interleukin-2 receptor expression in normal human lymphocytes. Int J Immunopharmacol. 1989;17:789–800. doi: 10.1016/0192-0561(89)90133-1.
- Characterization of the immunoregulatory properties of thymosin alpha 1 on interleukin-2 production and interleukin-2 receptor expression in normal human lymphocytesThymosin alpha 1 (Tα1) and thymosin fraction 5 (TF5) enhance interleukin-2 (IL-2) production and IL-2 receptor (IL-2R) expression in T-cells during early activation by mitogens like phytohemagglutinin (PHA). This effect does not require macrophages during thymosin preincubation but depends on macrophage-derived interleukin-1 beta (IL-1β) during subsequent mitogen exposure. Both helper (CD4+) and cytotoxic (CD8+) T-cell populations are direct targets of thymosin activity, underscoring their role in modulating immune responses and elucidating mechanisms underlying Tα1’s immunoregulatory effects.You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/0192056189901331?via%3Dihub.
Romani L, Bistoni F, Montagnoli C, Gaziano R, Bozza S, Bonifazi P, Zelante T, Moretti S, Rasi G, Garaci E, Puccetti P. Thymosin alpha1: an endogenous regulator of inflammation, immunity, and tolerance. Ann N Y Acad Sci. 2007;17:326–338. doi: 10.1196/annals.1415.002.
- Thymosin alpha1: an endogenous regulator of inflammation, immunity, and toleranceThymosin alpha 1 (Tα1), widely used to treat immunodeficiencies, malignancies, and infections, plays a central role in modulating dendritic cell (DC) function, crucial for balancing immunity and tolerance. Tα1 primes DCs for antifungal Th1 resistance, activates plasmacytoid DCs for antiviral responses via TLR/MyD88 pathways, and induces indoleamine 2,3-dioxygenase activity, promoting transplantation tolerance and reducing inflammatory allergy. Produced by cleavage of prothymosin alpha in various tissues, Tα1 serves as an endogenous immune regulator, offering potential for immunotherapy to manage inflammation, immunity, and tolerance across diverse clinical settings.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1196/annals.1415.002.
Pierluigi B, D’Angelo C, Fallarino F, Moretti S, Zelante T, Bozza S, De Luca A, Bistoni F, Garaci E, Romani L. Thymosin alpha1: the regulator of regulators? Ann N Y Acad Sci. 2010;17:1–5. doi: 10.1111/j.1749-6632.2010.05465.x.
- Thymosin alpha1: the regulator of regulators?The peripheral immune system balances immunity and tolerance through mechanisms like regulatory T cells (Treg), which are crucial for immunological tolerance. Dysfunctions in Treg cells are linked to chronic inflammatory and autoimmune diseases. Thymosin alpha 1 (Tα1), a thymic peptide, influences adaptive immunity by modulating innate immune receptor signals on dendritic cells, affecting T-helper cell effector and regulatory functions. Understanding Tα1’s molecular mechanisms could enhance vaccine development and immunomodulatory therapies.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1111/j.1749-6632.2010.05465.x.
Zhang Y, Chen H, Li YM, Zheng SS, Chen YG, Li LJ, Zhou L, Xie HY, Praseedom RK. Thymosin alpha1- and ulinastatin-based immunomodulatory strategy for sepsis arising from intra-abdominal infection due to carbapenem-resistant bacteria. J Infect Dis. 2008;17:723–730. doi: 10.1086/590500.
- Thymosin alpha1- and ulinastatin-based immunomodulatory strategy for sepsis arising from intra-abdominal infection due to carbapenem-resistant bacteriaA prospective, randomized study evaluated the efficacy of combining thymosin alpha 1 (Tα1) and ulinastatin with carbapenem therapy (CTU group) versus carbapenems and placebo (CP group) in 120 sepsis patients infected with carbapenem-resistant bacteria. The CTU group showed improved organ failure scores, better CD4+CD8+ counts, balanced pro- and anti-inflammatory cytokine levels, and significantly higher cumulative survival rates at 28, 60, and 90 days. While results suggest this combination therapy enhances survival, the study’s small sample size underscores the need for larger trials to confirm these findings.You can read the abstract of the article at https://academic.oup.com/jid/article-abstract/198/5/723/866603?redirectedFrom=fulltext&login=false.
Wang X, Li W, Niu C, Pan L, Li N, Li J. Thymosin alpha 1 is associated with improved cellular immunity and reduced infection rate in severe acute pancreatitis patients in a double-blind randomized control study. Inflammation. 2011;17:198–202. doi: 10.1007/s10753-010-9224-1.
- Thymosin alpha 1 is associated with improved cellular immunity and reduced infection rate in severe acute pancreatitis patients in a double-blind randomized control studyA double-blinded pilot trial evaluated the impact of thymosin alpha 1 (Tα1) on immunomodulation and outcomes in 24 severe acute pancreatitis (SAP) patients. Patients receiving Tα1 (3.2 mg twice daily for 7 days) showed faster recovery in monocyte HLA-DR expression, improved CD4/CD8 ratios, lower infection rates, and shorter ICU stays compared to conventional therapy. These findings suggest Tα1 enhances cell-mediated immunity and reduces complications in SAP, though larger studies are needed to confirm its benefits.You can read the abstract of the article at https://link.springer.com/article/10.1007/s10753-010-9224-1.
King R, Tuthill C. Immune Modulation with Thymosin Alpha 1 Treatment. VitamHorm. 2016;102:151-78.
- Immune Modulation with Thymosin Alpha 1 TreatmentThymosin alpha 1 (Tα1), originally isolated for its ability to restore immune function, has a broad mechanism of action that enhances multiple immune cell subsets involved in immune suppression. By activating Toll-like receptors on myeloid and plasmacytoid dendritic cells, Tα1 stimulates signaling pathways and cytokine production. Its immune-stimulating effects show promise for treating immune suppression associated with aging, infections, and cancer. Preclinical and clinical studies highlight its potential to improve immune cell function and treat various diseases.You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0083672916300036?via%3Dihub.
Milenkovic L, Mccann SM. Effects of thymosin alpha-1 on pituitary hormone release. Neuroendocrinology. 1992;55(1):14-9.
- Effects of thymosin alpha-1 on pituitary hormone releaseThymosins, including thymosin alpha 1 (Tα1), are thymic-derived peptides that regulate immune and hormonal functions. This study explored Tα1’s effects on pituitary hormone release in male rats. Intracerebroventricular injection of Tα1 reduced plasma levels of thyrotropin (TSH), adrenocorticotropin (ACTH), and prolactin (Prl), with no effect on growth hormone (GH). In vitro, Tα1 stimulated dose-dependent release of TSH and ACTH but did not influence Prl or GH, indicating both central and pituitary-level regulatory roles.You can read the abstract of the article at https://karger.com/nen/article-abstract/55/1/14/209073/Effects-of-Thymosin-Alpha-1-on-Pituitary-Hormone?redirectedFrom=fulltext.
hang, C., Zhou, J., Cai, K., Zhang, W., Liao, C., & Wang, C. (2018). Gene cloning, expression and immune adjuvant properties of the recombinant fusion peptide Tα1-BLP on avian influenza inactivate virus vaccine. Microbial pathogenesis, 120, 147–154. https://doi.org/10.1016/j.micpath.2018.05.003.
- Gene cloning, expression and immune adjuvant properties of the recombinant fusion peptide Tα1-BLP on avian influenza inactivate virus vaccineThymosin α1-bursin-like peptide (Tα1-BLP) is a novel immunopotentiator and vaccine adjuvant. In chickens immunized with Tα1-BLP combined with an H9N2 avian influenza inactivated virus vaccine, it enhanced antibody titers (HI, IgG, and neutralizing antibodies), stimulated Th1 (IFN-γ) and Th2 (IL-4) cytokine secretion, and promoted T and B lymphocyte proliferation. Viral challenge experiments showed reduced viral loads and lung damage, demonstrating Tα1-BLP’s protective efficacy. These findings suggest Tα1-BLP as an effective adjuvant for H9N2 avian influenza vaccines.You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0882401017315279?via%3Dihub.
Pei, F., Guan, X., & Wu, J. (2018). Thymosin alpha 1 treatment for patients with sepsis. Expert opinion on biological therapy, 18(sup1), 71–76. https://doi.org/10.1080/14712598.2018.1484104.
- Thymosin alpha 1 treatment for patients with sepsisThymosin alpha 1 (Tα1) is a promising immunomodulatory therapy for sepsis, capable of activating and restoring dysregulated immune responses. Clinical studies have shown that Tα1, alone or combined with anti-inflammatory treatments, can reduce sepsis mortality, enhance monocyte HLA-DR expression, and lower secondary infection rates. However, due to the heterogeneity of sepsis, these findings cannot be generalized to all patients. Future trials should focus on immunosuppressed septic patients to better evaluate Tα1’s therapeutic potential.You can read the abstract of the article at https://www.tandfonline.com/doi/full/10.1080/14712598.2018.1484104.
Wang F, Yu T, Zheng H, Lao X. Thymosin Alpha1-Fc Modulates the Immune System and Down-regulates the Progression of Melanoma and Breast Cancer with a Prolonged Half-life. Sci Rep. 2018;8(1):12351. Published 2018 Aug 17. doi:10.1038/s41598-018-30956-y.
- Thymosin Alpha1-Fc Modulates the Immune System and Down-regulates the Progression of Melanoma and Breast Cancer with a Prolonged Half-lifeThymosin alpha 1-Fc (Tα1-Fc), a fusion protein combining Tα1 with the Fc domain of human IgG4, exhibits significantly extended serum half-life (25 hours, 13 times longer than Tα1 alone) and enhanced therapeutic efficacy. Engineered to improve immune function, Tα1-Fc demonstrated potent antitumor effects in mouse models of 4T1 and B16F10 tumors by increasing lymphocyte numbers, upregulating CD86 expression, promoting IFN-γ and IL-2 secretion, and boosting tumor-infiltrating CD4+ and CD8+ T cells. By enhancing the activity and numbers of T cells, these findings highlight the potential of Tα1-Fc as an advanced immunotherapeutic agent for cancer treatment.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC6097990/.
Matteucci, C., Grelli, S., Balestrieri, E., Minutolo, A., Argaw-Denboba, A., Macchi, B., Sinibaldi-Vallebona, P., Perno, C. F., Mastino, A., & Garaci, E. (2017). Thymosin alpha 1 and HIV-1: recent advances and future perspectives. Future microbiology, 12, 141–155. https://doi.org/10.2217/fmb-2016-0125.
- Thymosin alpha 1 and HIV-1: recent advances and future perspectivesThymosin alpha 1 (Tα1) shows promise in addressing incomplete immune reconstitution in HIV-1 patients on antiretroviral therapy, which is often marked by immunological unresponsiveness, persistent inflammation, and poor cytotoxic T-cell responses. Acting as a multitasking protein, Tα1 helps restore immune homeostasis across various conditions, including infections, cancer, and aging, by modulating immune dysfunction and inflammation. This review highlights the current in vitro and in vivo evidence of Tα1’s potential in HIV-1 treatment and explores future therapeutic prospects.You can read the abstract of the article at https://www.tandfonline.com/doi/full/10.2217/fmb-2016-0125.
Matteucci, C., Minutolo, A., Pollicita, M., Balestrieri, E., Grelli, S., D’Ettorre, G., Vullo, V., Bucci, I., Luchini, A., Aquaro, S., Sinibaldi-Vallebona, P., Macchi, B., Perno, C. F., Mastino, A., & Garaci, E. (2015). Thymosin α 1 potentiates the release by CD8(+) cells of soluble factors able to inhibit HIV-1 and human T lymphotropic virus 1 infection in vitro. Expert opinion on biological therapy, 15 Suppl 1, S83–S100. https://doi.org/10.1517/14712598.2015.1021677.
- Thymosin α 1 potentiates the release by CD8(+) cells of soluble factors able to inhibit HIV-1 and human T lymphotropic virus 1 infection in vitroThymosin α-1 (Tα1) enhances the release of antiretroviral soluble factors from LPS-stimulated CD8(+) cells, effectively inhibiting in vitro HIV-1 infection in monocyte-derived macrophages (MDMs) and PBMCs, as well as HTLV-1 infection in PBMCs. In PBMCs from HIV(+) individuals, Tα1 induces a distinct transcriptional response, suggesting its potential as a complementary approach in antiretroviral therapy, innovative treatments, and vaccine strategies.You can read the full article at https://www.tandfonline.com/doi/full/10.1517/14712598.2015.1021677.
Shrivastava P, Singh SM, Singh N. Activation of tumor-associated macrophages by thymosin alpha 1. Int J ImmunopatholPharmacol. 2004;17(1):39-47.
- Activation of tumor-associated macrophages by thymosin alpha 1This study demonstrates that thymosin alpha 1 (Tα1) can activate tumor-associated macrophages (TAM) in mice bearing Dalton’s lymphoma (DL) to a tumoricidal state. Tα1 treatment enhanced TAM functions, including interleukin-1 and tumor necrosis factor production, reactive oxygen intermediates and nitric oxide generation, as well as pinocytosis, phagocytosis, antigen presentation, and tumor cytotoxicity. These findings highlight the potential of Tα1 to overcome immune suppression in T-cell lymphoma by activating TAM.You can read the abstract of the article at https://journals.sagepub.com/doi/10.1177/039463200401700106?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Garaci E, Pica F, Serafino A, et al. Thymosin α1 and cancer: action on immune effector and tumor target cells. Ann N Y Acad Sci. 2012;1269:26-33.
- Thymosin α1 and cancer: action on immune effector and tumor target cellsThymosin alpha 1 (Tα1) is a versatile immune modulator that enhances T cell and natural killer cell maturation, cytokine production, and cytotoxic T lymphocyte responses. It also increases the expression of major histocompatibility complex class I molecules and tumor antigens in both experimental and human tumor cell lines, contributing to its antitumor activity by boosting immune recognition and response against tumors.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1111/j.1749-6632.2012.06697.x.
Liang YR, Guo Z, Jiang JH, Xiang BD, Li LQ. Thymosin α1 therapy subsequent to radical hepatectomy in patients with hepatitis B virus-associated hepatocellular carcinoma: A retrospective controlled study. OncolLett. 2016;12(5):3513–3518. doi:10.3892/ol.2016.5121.
- Thymosin α1 therapy subsequent to radical hepatectomy in patients with hepatitis B virus-associated hepatocellular carcinoma: A retrospective controlled studyThymosin α1 (Tα1) therapy following radical hepatectomy significantly improves liver function and enhances outcomes in patients with HBV-associated hepatocellular carcinoma (HCC). A retrospective study with propensity score matching showed that patients receiving Tα1 therapy had higher 1-, 2-, and 3-year overall survival (87.2%, 82.0%, 68.4%) and recurrence-free survival rates (79.7%, 70.8%, 67.3%) compared to controls, indicating its potential to reduce recurrence and improve survival in this population.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC5103975/.
Garaci E, Pica F, Serafino A, Balestrieri E, Matteucci C, Moroni G, Sorrentino R, Zonfrillo M, Pierimarchi P, Sinibaldi-Vallebona P. Thymosin α1 and cancer: Action on immune effector and tumor target cells. Ann N Y Acad Sci. 2012;1269:26–33. doi: 10.1111/j.1749-6632.2012.06697.x.
- Thymosin α1 and cancer: Action on immune effector and tumor target cellsThymosin alpha 1 (Tα1) exhibits broad immunomodulatory effects, particularly on T cells and natural killer cells, enhancing cytokine production and cytotoxic responses. It also upregulates major histocompatibility complex class I molecules and tumor antigen expression in tumor cell lines, boosting immune recognition. Additionally, Tα1 has been shown to influence the microenvironment of tumor cells, making them more susceptible to immune attack. These properties highlight Tα1’s potential to enhance antitumor activity through both immune modulation and direct effects on tumor cells, ultimately improving therapeutic outcomes against tumor cells.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1111/j.1749-6632.2012.06697.x.
Cheng SQ, Wu MC, Chen H, Shen F, Yang JH, Zhao YX, Mo ZW. Influence of thymosin α1 on postoperative recurrence of primary liver cancer. Chin J Hepatobil Surg. 2004;10:592–593.
Palmieri G, Biondi E, Morabito A, Rea A, Bianco A. Could thymostimulin prevent hepatocellular carcinoma occurrence in patients with liver cirrhosis? Oncol Rep. 1996;3:655–656.
- Could thymostimulin prevent hepatocellular carcinoma occurrence in patients with liver cirrhosis?In a study of 34 liver cirrhosis patients with chronic hepatitis B or C, thymostimulin treatment (50 mg/m², three times weekly) was associated with a significant reduction in hepatocellular carcinoma (HCC) occurrence compared to expected rates (p<0.05) over a median follow-up of six years. The treatment was well-tolerated, suggesting that immunomodulatory therapy may help lower HCC risk in cirrhotic patients with chronic hepatitis B. Additionally, patients with chronic hepatitis B who received thymostimulin therapy showed improved outcomes. This study underscores the potential of immunomodulatory treatments for patients with chronic hepatitis B in reducing HCC risk. Given the burden of chronic hepatitis B in cirrhotic patients, these findings offer promising therapeutic insights. Further research on thymostimulin for chronic hepatitis B patients is warranted to confirm its potential benefits.You can read the abstract of the article at https://www.spandidos-publications.com/or/3/4/655.
Wolf E, Milazzo S, Boehm K, Zwahlen M, Horneber M. Thymic peptides for treatment of cancer patients. Cochrane Database Syst Rev. 2011;(2):CD003993.
- Thymic peptides for treatment of cancer patientsA meta-analysis of 26 trials (2736 cancer patients) evaluating purified thymus extracts (pTE) and synthetic thymic peptides (sTP) alongside chemotherapy or radiotherapy found no significant benefits for overall survival, disease-free survival, or tumor response rates. However, pTE showed a reduced risk of severe infectious complications (RR 0.54, p=0.0008) during treatment, and thymosin α1 suggested a potential trend towards reduced mortality and improved DFS. Both pTE and sTP were well-tolerated, though most trials had a moderate risk of bias, limiting definitive conclusions.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC6481824/.
Lee D, Kim SS, Seong S, Cho W, Yu H. Stage IV Wilms Tumor Treated by Korean Medicine, Hyperthermia and Thymosin-α1: A Case Report. Case Rep Oncol. 2016;9(1):119-25.
- Stage IV Wilms Tumor Treated by Korean Medicine, Hyperthermia and Thymosin-α1: A Case ReportThis case study reports on the successful use of integrative medical therapy combining hyperthermia, thymosin-α1 (Zadaxin), and herbal remedies for a 4th-phase Wilms tumor with liver and lung metastases. Treatment led to remission of liver metastases and stable maintenance of lung lesions without progression. The findings suggest that integrative approaches, including hyperthermia and thymosin-α1, may offer a promising complementary option for Wilms tumor patients unresponsive to conventional therapies like surgery, chemotherapy, and radiotherapy.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4899649/.
Guo Y, Chang H, Li J, et al. Thymosin alpha 1 suppresses proliferation and induces apoptosis in breast cancer cells through PTEN-mediated inhibition of PI3K/Akt/mTOR signaling pathway. Apoptosis. 2015;20(8):1109-21.
- Thymosin alpha 1 suppresses proliferation and induces apoptosis in breast cancer cells through PTEN-mediated inhibition of PI3K/Akt/mTOR signaling pathwayThymosin alpha 1 (Tα1) inhibits breast cancer cell growth by upregulating the tumor suppressor gene PTEN, which suppresses the PI3K/Akt/mTOR signaling pathway and induces apoptosis. This effect is more pronounced in PTEN-expressing cells, while PTEN knockdown reverses Tα1’s growth inhibition. Tα1 enhances mitochondrial apoptosis by upregulating Bax and cleaved caspase-3/9 and downregulating Bcl-2, demonstrating a synergistic potential for targeting PI3K/Akt/mTOR in breast cancer treatment.You can read the abstract of the article at https://link.springer.com/article/10.1007/s10495-015-1138-9.
Garaci E, Pica F, Rasi G, Favalli C. Thymosin alpha 1 in the treatment of cancer: from basic research to clinical application. Int J Immunopharmacol. 2000;22(12):1067-76.
- Thymosin alpha 1 in the treatment of cancer: from basic research to clinical applicationCombining thymosin alpha 1 (Tα1) with low doses of interferon (IFN) or interleukin (IL)-2 has been shown to effectively restore immune responses suppressed by tumor growth or chemotherapy. This approach enhances the anti-tumor effects of chemotherapy while significantly reducing its toxicity. Studies highlight the potential of this chemo-immunotherapeutic strategy for improving cancer treatment outcomes in both experimental and human cases.You can read the abstract of the article at https://www.sciencedirect.com/science/article/abs/pii/S0192056100000758?via%3Dihub.
Shrivastava P, Singh SM, Singh N. Effect of thymosin alpha 1 on the antitumor activity of tumor-associated macrophage-derived dendritic cells. J Biomed Sci. 2004;11(5):623-30.
- Effect of thymosin alpha 1 on the antitumor activity of tumor-associated macrophage-derived dendritic cellsThymosin alpha 1 (Tα1) enhances the differentiation of tumor-associated macrophages (TAM) into dendritic cells (DC) with the aid of GM-CSF, IL-4, and TNF, improving their antitumor activity in a murine model of Dalton’s lymphoma. DC derived from Tα1-treated TAM produce higher levels of cytokines like IL-1 and TNF-alpha and exhibit increased antitumor effects. Adoptive immunotherapy using these DC significantly delays tumor growth and prolongs survival, highlighting Tα1’s potential in enhancing DC-mediated antitumor responses.You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/15316138/.
Shen, X., Li, Q., Wang, F., Bao, J., Dai, M., Zheng, H., & Lao, X. (2018). Generation of a novel long-acting thymosin alpha1-Fc fusion protein and its efficacy for the inhibition of breast cancer in vivo. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 108, 610–617. https://doi.org/10.1016/j.biopha.2018.09.064.
- Generation of a novel long-acting thymosin alpha1-Fc fusion protein and its efficacy for the inhibition of breast cancer in vivoThymosin alpha 1 fused with the Fc domain of human IgG1 (Tα1-Fc) is a novel long-acting protein with enhanced antitumor activity and immune modulation compared to Tα1 alone. Tα1-Fc effectively inhibited the growth of breast cancer cells in vivo, increased CD4+ and CD8+ T cell levels, and elevated interferon-γ and interleukin-2 levels in treated mice. Additionally, it mitigated immunosuppression caused by hydrocortisone, demonstrating its potential as a powerful strategy for boosting immune responses against tumors.You can read the full article at https://www.sciencedirect.com/science/article/pii/S0753332218342124?via%3Dihub.
Maio, M., Mackiewicz, A., Testori, A., Trefzer, U., Ferraresi, V., Jassem, J., Garbe, C., Lesimple, T., Guillot, B., Gascon, P., Gilde, K., Camerini, R., Cognetti, F., & Thymosin Melanoma Investigation Group (2010). Large randomized study of thymosin alpha 1, interferon alfa, or both in combination with dacarbazine in patients with metastatic melanoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 28(10), 1780–1787. https://doi.org/10.1200/JCO.2009.25.5208.
- Large randomized study of thymosin alpha 1, interferon alfa, or both in combination with dacarbazine in patients with metastatic melanomaA large randomized study evaluated the efficacy and safety of combining thymosin alpha 1 (Tα1) with dacarbazine (DTIC) and interferon-alpha (IFN-α) in metastatic melanoma patients. Tα1 significantly improved tumor response rates and extended the duration of response (1.9–23.2 months) compared to the control group (4.4–8.4 months). Median overall survival (OS) increased from 6.6 months in the control group to 9.4 months in the Tα1-treated groups, with a trend toward better progression-free survival (PFS). Importantly, adding Tα1 did not increase toxicity, supporting its potential for further clinical evaluation in metastatic melanoma.You can read the full article at https://ascopubs.org/doi/10.1200/JCO.2009.25.5208?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed.
Kharazmi-Khorassani, J., & Asoodeh, A. (2019). Thymosin alpha-1; a natural peptide inhibits cellular proliferation, cell migration, the level of reactive oxygen species and promotes the activity of antioxidant enzymes in human lung epithelial adenocarcinoma cell line (A549). Environmental toxicology, 34(8), 941–949. https://doi.org/10.1002/tox.22765.
- Thymosin alpha-1; a natural peptide inhibits cellular proliferation, cell migration, the level of reactive oxygen species and promotes the activity of antioxidant enzymes in human lung epithelial adenocarcinoma cell line (A549).This study examined the effects of thymosin alpha-1 (Thα1) on human lung cancer A549 cells, revealing an anti-proliferative effect at specific concentrations (24 and 48 μg/ml). Thα1 demonstrated significant antioxidant activity by enhancing catalase, superoxide dismutase, and glutathione peroxidase levels while reducing reactive oxygen species (ROS). It also inhibited cell migration in a concentration-dependent manner but showed no significant induction of apoptosis. These findings highlight the antioxidant properties of Thα1 in lung cancer cells.You can read the abstract of the article at https://onlinelibrary.wiley.com/doi/10.1002/tox.22765.
Danielli, R., Fonsatti, E., Calabrò, L., Di Giacomo, A. M., & Maio, M. (2012). Thymosin α1 in melanoma: from the clinical trial setting to the daily practice and beyond. Annals of the New York Academy of Sciences, 1270, 8–12. https://doi.org/10.1111/j.1749-6632.2012.06757.x.
- Thymosin α1 in melanoma: from the clinical trial setting to the daily practice and beyondInsert the keyword “clinical trials” four times Thymosin α1 (Tα1), an immunomodulatory peptide first identified in 1977, has shown promise in treating immune deficiencies and cancer, including melanoma. Clinical trials, particularly a large randomized phase II study combining Tα1 with dacarbazine and interferon alpha in metastatic melanoma patients, have demonstrated its safety and potential efficacy. These findings provide a basis for exploring Tα1’s therapeutic applications in melanoma further.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1111/j.1749-6632.2012.06757.x
Goldstein, A. L., & Goldstein, A. L. (2009). From lab to bedside: emerging clinical applications of thymosin alpha 1. Expert opinion on biological therapy, 9(5), 593–608. https://doi.org/10.1517/14712590902911412.
- From lab to bedside: emerging clinical applications of thymosin alpha 1Thymosin alpha 1 (Tα1), a synthetic thymic peptide, is approved in over 35 countries for treating hepatitis B and C and as an immune stimulant. In late-stage trials for hepatitis C and stage IV melanoma, Tα1 shows broader potential in addressing diseases like septic shock, acute respiratory distress syndrome, peritonitis, cytomegalovirus, TB, SARS, and severe lung infections. It also demonstrates promise as a chemoprotective agent during chemotherapy, expanding its clinical relevance.You can read the abstract of the article at https://www.tandfonline.com/doi/full/10.1517/14712590902911412.
Malinda KM, Sidhu GS, Banaudha KK, et al. Thymosin alpha 1 stimulates endothelial cell migration, angiogenesis, and wound healing. J Immunol. 1998;160(2):1001-6.
- Thymosin alpha 1 stimulates endothelial cell migration, angiogenesis, and wound healingThymosin alpha 1 (Tα1), a peptide derived from the thymus, enhances endothelial cell migration, angiogenesis, and wound healing. In vitro, it acts as a potent chemoattractant for endothelial cells and monocytes, promoting cell differentiation. In vivo studies showed Tα1 stimulates angiogenesis and accelerates wound repair when administered topically or intraperitoneally, highlighting its therapeutic potential in wound healing.You can read the full article at https://pubmed.ncbi.nlm.nih.gov/9551940/.
Available from https://www.federallabs.org/technology/thymosin-alpha-1-promotes-tissue-repair-angiogenesis-and-cell-migration.
Wang, G., He, F., Xu, Y., Zhang, Y., Wang, X., Zhou, C., Huang, Y., & Zou, J. (2017). Immunopotentiator Thymosin Alpha-1 Promotes Neurogenesis and Cognition in the Developing Mouse via a Systemic Th1 Bias. Neuroscience bulletin, 33(6), 675–684. https://doi.org/10.1007/s12264-017-0162-x.
- Immunopotentiator Thymosin Alpha-1 Promotes Neurogenesis and Cognition in the Developing Mouse via a Systemic Th1 BiasThis study found that peripherally administered thymosin alpha-1 (Ta1) in neonatal mice enhanced cognitive abilities and hippocampal neurogenesis. Ta1 treatment increased markers of neurogenesis and neurotrophic factors while reducing pro-inflammatory cytokines like IL-6 and TNF-α, promoting a Th1-biased immune response. Additionally, Ta1 protected against lipopolysaccharide-induced neurodevelopmental impairments, suggesting its potential role in fostering brain development and cognitive function through immune modulation and neuroprotection.You can read the abstract of the article at https://pmc.ncbi.nlm.nih.gov/articles/PMC5725380/.
Day, P., & Duggal, M. (2010). Interventions for treating traumatised permanent front teeth: avulsed (knocked out) and replanted. The Cochrane database of systematic reviews, (1), CD006542. https://doi.org/10.1002/14651858.CD006542.pub2.
- Interventions for treating traumatised permanent front teeth: avulsed (knocked out) and replantedThis Cochrane review update evaluated interventions for managing avulsed and replanted permanent front teeth, but the evidence remains insufficient and of very low quality. Four studies involving 183 participants assessed different interventions, including hyperbaric oxygen, root canal medicaments, extra- or intra-oral endodontics, and thymosin alpha 1. Some interventions, such as hyperbaric oxygen and thymosin alpha 1, showed potential benefits for periodontal healing and tooth survival, but the results were uncertain due to high risk of bias and imprecision. Further high-quality randomized controlled trials are urgently needed to establish effective treatment strategies.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC6363052/.
Yang X, Chen Y, Zhang J, et al. Thymosin α1 treatment reduces hepatic inflammation and inhibits hepatocyte apoptosis in rats with acute liver failure. ExpTher Med. 2018;15(4):3231–3238. doi:10.3892/etm.2018.5843.
- Thymosin α1 treatment reduces hepatic inflammation and inhibits hepatocyte apoptosis in rats with acute liver failureThis study evaluated thymosin α1 (Tα1) in a rat model of acute liver failure (ALF) and found that Tα1 significantly improved survival rates by enhancing immunofunction and reducing hepatocyte apoptosis. Tα1 treatment lowered plasma ALT, AST, TBIL, and TNF-α levels while increasing IL-10 levels compared to untreated ALF rats. Histological analysis showed less hepatocyte necrosis and fewer apoptotic cells in Tα1-treated rats, with a lower Bax-to-Bcl-2 ratio indicating reduced apoptosis. These findings suggest Tα1 mitigates hepatic inflammation and cell death, improving outcomes in ALF.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC5840938/.
Romani L, Bistoni F, Gaziano R, Bozza S, Montagnoli C, Perruccio K, Pitzurra L, Bellocchio S, Velardi A, Rasi G, et al. Thymosin alpha 1 activates dendritic cells for antifungal Th1 resistance through toll-like receptor signaling. Blood. 2004;103:4232–4239. doi: 10.1182/blood-2003-11-4036.
- Thymosin alpha 1 activates dendritic cells for antifungal Th1 resistance through toll-like receptor signalingThymosin alpha 1 (Tα1) enhances dendritic cell (DC) maturation and interleukin-12 production in response to Aspergillus fumigatus through a p38 MAPK/NF-κB pathway involving Toll-like receptors. In vivo, Tα1 activates Th1-dependent antifungal immunity, accelerates myeloid recovery, and protects immunocompromised mice from aspergillosis. These findings highlight Tα1’s potential as a therapeutic adjuvant to coordinate innate and adaptive immune responses against fungal infections.You can read the full article at https://www.sciencedirect.com/science/article/pii/S0006497120554207?via%3Dihub.
Bozza S, Gaziano R, Bonifazi P, Zelante T, Pitzurra L, Montagnoli C, Moretti S, Castronari R, Sinibaldi P, Rasi G, et al. Thymosin alpha1 activates the TLR9/MyD88/IRF7-dependent murine cytomegalovirus sensing for induction of anti-viral responses in vivo. IntImmunol. 2007;19:1261–1270. doi: 10.1093/intimm/dxm097.
- Thymosin alpha1 activates the TLR9/MyD88/IRF7-dependent murine cytomegalovirus sensing for induction of anti-viral responses in vivoThymosin alpha 1 (Tα1) protects mice from murine cytomegalovirus (MCMV) infection by activating plasmacytoid dendritic cells via TLR9 and MyD88-dependent viral sensing. This triggers IFN regulatory factor 7, enhancing IFN-α/IFN-γ-dependent antiviral immunity. These findings highlight Tα1’s potential as an immune adjuvant for combating cytomegalovirus infections.You can read the abstract of the article at https://academic.oup.com/intimm/article-abstract/19/11/1261/786352?redirectedFrom=fulltext&login=false.
Yang X, Qian F, He HY, Liu KJ, Lan YZ, Ni B, Tian Y, Fu XL, Zhang J, Shen ZG, et al. Effect of thymosin alpha-1 on subpopulations of Th1, Th2, Th17, and regulatory T cells (Tregs) in vitro. Braz J Med Biol Res. 2012;45:25–32. doi: 10.1590/S0100-879X2011007500159.
- Effect of thymosin alpha-1 on subpopulations of Th1, Th2, Th17, and regulatory T cells (Tregs) in vitroxInsert the keyword “t cells” four times Thymosin alpha 1 (Tα1) modulates immune responses in gastric carcinoma by increasing the percentage of CD4+CD25+Foxp3+ regulatory T cells (Tregs) and the production of IL-1β, TNF-α, and IL-6 in peripheral blood mononuclear cells (PBMCs) from patients. These findings suggest Tα1’s potential as an immunoregulatory factor in managing immune responses in gastric cancer.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC3854146/.
Nakama T, Hirono S, Moriuchi A, Hasuike S, Nagata K, Hori T, Ido A, Hayashi K, Tsubouchi H. Etoposide prevents apoptosis in mouse liver with D-galactosamine/lipopolysaccharide-induced fulminant hepatic failure resulting in reduction of lethality. Hepatology. 2001;33:1441–1450. doi: 10.1053/jhep.2001.24561.
- Etoposide prevents apoptosis in mouse liver with D-galactosamine/lipopolysaccharide-induced fulminant hepatic failure resulting in reduction of lethalityEtoposide effectively reduces D-galactosamine (GalN)/lipopolysaccharide (LPS)-induced fulminant hepatic failure in mice by decreasing hepatocyte apoptosis and mortality. While it does not alter serum TNF-alpha levels or TNFR1 expression, etoposide enhances Bcl-xL, an anti-apoptotic molecule, and lowers caspase-3 activity. These findings highlight etoposide’s potential therapeutic role in TNF-alpha-mediated liver diseases.You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/11391533/.
Chastre A, Belanger M, Beauchesne E, Nguyen BN, Desjardins P, Butterworth RF. Inflammatory cascades driven by tumor necrosis factor-alpha play a major role in the progression of acute liver failure and its neurological complications. PLoS One. 2012;7:e49670. doi: 10.1371/journal.pone.0049670.
- Inflammatory cascades driven by tumor necrosis factor-alpha play a major role in the progression of acute liver failure and its neurological complicationsThis study demonstrates that etanercept, a TNF-α neutralizing molecule, significantly delays the progression of hepatic encephalopathy (HE) and mitigates liver injury in a mouse model of acute liver failure (ALF) caused by azoxymethane (AOM). Administered within three hours of injury, etanercept reduces hepatic necrosis, plasma ammonia, and inflammation markers (IL-6 and CD40L) while attenuating brain inflammation and microglial activation. These findings suggest etanercept’s potential as a therapeutic strategy for managing ALF and HE in patients awaiting liver transplantation.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC3499491/.
Wang K. Molecular mechanisms of hepatic apoptosis. Cell Death Dis. 2014;5:e996. doi: 10.1038/cddis.2013.499.
- Molecular mechanisms of hepatic apoptosisApoptosis plays a key role in liver diseases, triggered by factors like alcohol, viruses, toxic bile acids, fatty acids, drugs, and immune responses. It involves interconnected pathways, including death receptor signaling, ROS generation, ER stress, lysosomal permeabilization, and mitochondrial dysfunction, with one pathway potentially dominating at different stages. The progression of liver disease depends on the balance between pro-apoptotic and anti-apoptotic mechanisms, making a clear understanding of these pathways critical for developing effective therapeutic strategies.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4040708/.
Zhang P, Shen H, Huang J, Wang H, Zhang B, Zhou R, Zhong B, Fan X. Intraperitoneal administration of fetuin-A attenuates D-galactosamine/lipopolysaccharide-induced liver failure in mouse. Dig Dis Sci. 2014;59:1789–1797. doi: 10.1007/s10620-014-3071-0.
- Intraperitoneal administration of fetuin-A attenuates D-galactosamine/lipopolysaccharide-induced liver failure in mouseFetuin-A, an anti-inflammatory protein, was found to protect against D-galactosamine/lipopolysaccharide (D-GalN/LPS)-induced fulminant hepatic failure (FHF) in mice. FHF reduced fetuin-A expression in liver tissue, while pre-treatment with exogenous fetuin-A improved liver function, decreased inflammatory markers (TNF-α and IL-6), reduced hepatocyte apoptosis, and lowered mortality rates. These findings suggest fetuin-A as a potential therapeutic agent for FHF by mitigating liver inflammation and cellular damage.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4119259/.
Romani L, Bistoni F, Montagnoli C, et al. Thymosin alpha1: an endogenous regulator of inflammation, immunity, and tolerance. Ann N Y Acad Sci. 2007;1112:326-38.
- Thymosin alpha1: an endogenous regulator of inflammation, immunity, and toleranceThymosin alpha1 (Tα1), a peptide first identified in 1972, plays a significant role in modulating immune responses through its effects on dendritic cells (DCs). By engaging Toll-like receptor (TLR)-dependent pathways, Tα1 primes DCs to enhance antifungal Th1 immunity, activates plasmacytoid DCs to bolster antiviral defenses via interferon pathways, and induces tolerogenic mechanisms such as tryptophan catabolism to support transplantation tolerance and mitigate allergies. Produced endogenously, Tα1 emerges as a key regulator of immune homeostasis, with potential for therapeutic applications in managing inflammation, immunity, and tolerance across diverse clinical conditions.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1196/annals.1415.002.
Romani, L., Oikonomou, V., Moretti, S., Iannitti, R. G., D’Adamo, M. C., Villella, V. R., Pariano, M., Sforna, L., Borghi, M., Bellet, M. M., Fallarino, F., Pallotta, M. T., Servillo, G., Ferrari, E., Puccetti, P., Kroemer, G., Pessia, M., Maiuri, L., Goldstein, A. L., & Garaci, E. (2017). Thymosin α1 represents a potential potent single-molecule-based therapy for cystic fibrosis. Nature medicine, 23(5), 590–600. https://doi.org/10.1038/nm.4305.
- Thymosin α1 represents a potential potent single-molecule-based therapy for cystic fibrosisCystic fibrosis (CF), primarily caused by the p.Phe508del mutation in the CFTR gene, leads to defective chloride channel activity and chronic lung inflammation, requiring multidrug therapies. Thymosin alpha 1 (Tα1), a naturally occurring polypeptide with a strong safety profile, has shown promise as a single-agent therapeutic for CF. In studies with CF mice and human cells, Tα1 reduced inflammation while enhancing CFTR protein maturation, stability, and activity, addressing both core defects and inflammatory complications of CF, highlighting its potential as a multifaceted treatment option.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC5420451/.
Xu, Y., Jiang, Y., Wang, L., Huang, J., Wen, J., Lv, H., Wu, X., Wan, C., Yu, C., Zhang, W., Zhao, J., Zhou, Y., & Chen, Y. (2019). Thymosin Alpha-1 Inhibits Complete Freund’s Adjuvant-Induced Pain and Production of Microglia-Mediated Pro-inflammatory Cytokines in Spinal Cord. Neuroscience bulletin, 35(4), 637–648. https://doi.org/10.1007/s12264-019-00346-z.
- Thymosin Alpha-1 Inhibits Complete Freund’s Adjuvant-Induced Pain and Production of Microglia-Mediated Pro-inflammatory Cytokines in Spinal CordThymosin alpha-1 (Tα1) has shown therapeutic potential in inflammatory pain by attenuating pain hypersensitivity induced by complete Freund’s adjuvant (CFA) in rodents. Tα1 reduced pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) in inflamed skin and spinal cord, inhibited microglial activation, and normalized the imbalance in vesicular neurotransmitter transporters (VGLUT and VGAT) in the spinal cord. These findings highlight Tα1’s role in modulating inflammation, neuroprotection, and pain regulation pathways.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC6616621/.
Carraro G, Naso A, Montomoli E, et al. Thymosin-alpha 1 (Zadaxin) enhances the immunogenicity of an adjuvated pandemic H1N1v influenza vaccine (Focetria) in hemodialyzed patients: a pilot study. Vaccine. 2012;30(6):1170-80.
- Thymosin-alpha 1 (Zadaxin) enhances the immunogenicity of an adjuvated pandemic H1N1v influenza vaccine (Focetria) in hemodialyzed patients: a pilot studyA pilot clinical trial in hemodialyzed patients assessed the impact of combining the adjuvanted H1N1 pandemic influenza vaccine with Thymosin alpha 1 (Tα1). Patients receiving the vaccine with Tα1 at two doses (3.2 mg and 6.4 mg) showed improved immune responses compared to those receiving the vaccine alone, meeting European licensing criteria for pandemic vaccines. Tα1 enhanced Geometric Mean Titers (GMT), Geometric Mean Ratios (GMR), and seroconversion rates without causing adverse events or altering hematology or chemistry values. These findings suggest Tα1 as a safe and effective adjuvant to boost influenza vaccine efficacy in immunosuppressed populations.You can read the full article at https://www.sciencedirect.com/science/article/abs/pii/S0264410X11019372?via%3Dihub.
Ershler WB, Gravenstein S, Geloo ZS. Thymosin alpha 1 as an adjunct to influenza vaccination in the elderly: rationale and trial summaries. Ann N Y Acad Sci. 2007;1112:375-84.
- Thymosin alpha 1 as an adjunct to influenza vaccination in the elderly: rationale and trial summariesImmune senescence in aging is typically mild but can be exacerbated by chronic conditions and their treatments, increasing susceptibility to infections and reducing vaccine efficacy, particularly in the elderly. Influenza vaccination, despite increased coverage, remains less effective in this population, contributing to significant morbidity and mortality. Thymosin alpha 1 (Tα1) has shown promise as an adjuvant to enhance vaccine responses in both animal models and human trials. These findings support further exploration of Tα1 to improve vaccine effectiveness in the elderly and in scenarios with limited antigen availability.You can read the abstract of the article at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1196/annals.1415.050.
Panatto D, Amicizia D, Lai PL, Camerini R, De rosa A, Gasparini R. Utility of thymosin alpha-1 (Zadaxin) as a co-adjuvant in influenza vaccines: a review. J Prev Med Hyg. 2011;52(3):111-5.
- Utility of thymosin alpha-1 (Zadaxin) as a co-adjuvant in influenza vaccines: a reviewInfluenza poses a significant health challenge, especially for the elderly and immunocompromised individuals, who often show poor responses to vaccination. To address this, adjuvated vaccines and immunostimulants like Thymosin alpha 1 (Tα1) have been explored to enhance vaccine efficacy. Tα1, a 28-amino-acid peptide, boosts T-cell, dendritic cell, and antibody responses and modulates cytokine and chemokine production. Studies suggest that Tα1 improves influenza vaccine performance in high-risk groups, offering promising prospects for more effective vaccination strategies, though further research on co-adjuvants is needed.You can read the abstract of the article at https://pubmed.ncbi.nlm.nih.gov/22010537/#:~:text=Talpha1%20is%20a%20biologically%20active,elderly%20and%20subjects%20at%20risk.
- Xu YG, Guan XT, Liu ZM, Tian CY, Cui LC. Immunogenicity in Swine of Orally Administered Recombinant Lactobacillus plantarum Expressing Classical Swine Fever Virus E2 Protein in Conjunction with Thymosin α-1 as an Adjuvant. Appl Environ Microbiol. 2015;81(11):3745-52.
- Immunogenicity in Swine of Orally Administered Recombinant Lactobacillus plantarum Expressing Classical Swine Fever Virus E2 Protein in Conjunction with Thymosin α-1 as an AdjuvantClassical swine fever (CSF), a highly contagious disease caused by CSFV, leads to significant economic losses in pig industries. This study evaluated genetically engineered Lactobacillus plantarum expressing the CSFV E2 protein alone (L. plantarum/pYG-E2) or combined with the immune-modifier Thymosin α-1 (Tα1) (L. plantarum/pYG-E2-Tα1) as oral vaccines. Both formulations effectively induced protective immunity in pigs, eliciting mucosal (IgA), humoral (IgG), and cellular (CTL) immune responses. Notably, L. plantarum/pYG-E2-Tα1 showed superior immunogenicity due to Tα1’s adjuvant effect, enhancing immune responsiveness and lymphocyte function. This approach offers a promising strategy for CSFV vaccine development.You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4421069/.
Patient Success Stories

Before
After

At the age of 60, I look and feel better than I ever have in my entire life! Switching my health program and hormone replacement therapy regimen over to Genemedics was one of the best decisions I’ve ever made in my life! Genemedics and Dr George have significantly improved my quality of life and also dramatically improved my overall health.
Nick Cassavetes ,60 yrs old Movie Director (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer

Before
After

I am now in my mid-sixties and feel better than I did in my 20’s. Many people have commented that I actually look 20 years younger since I started the program at Genemedics. Calling Dr. George has proven to be one of the best decisions I have made in my life. Doctors and society convince us that developing various health issues and negative sy...
Pamela Hill ,66 yrs old Actress (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer
What to expect during your consultation:
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have
Free Consultation
Start Your Journey to a Younger, Healthier You!
Categories
Information
Free Consultation
STEPS AWAY FROM A YOUNGER. HEALTHIER YOU!
Call 800-277-4041 for a Free Consultation
What to expect during your consultation:
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have