Peptides
- 5-amino-1MQ
- Aminophylline
- Aniracetam
- ARA 290
- Argireline + Leuphasyl
- BPC-157
- Bremelanotide
- Cerebrolysin
- CJC-1295
- Delta Sleep-Inducing Peptide
- Dihexa
- Elampretide (SS-31)
- Epithalon
- FG Loop Peptide (FGL)
- GHK-Cu
- Ginsenoside Rg3
- Glycyrrhetinic Acid
- Ipamorelin
- Kisspeptin
- KPV
- LL-37
- Melanotan 1
- Melanotan 2
- Mitochondrial ORF of the twelve S c (MOTS-c)
- MK-677 (IBUTAMOREN)
- Nicotinamide Adenine Dinucleotide (NAD+)
- Nicotinamide Riboside
- NMN (Nicotinamide Mononucleotide)
- Noopept
- Pegylated Mechano Growth Factor
- Selank
- Semax
- Sermorelin
- SRT2104
- Tesamorelin
- Thymosin Alpha 1
- Thymosin Beta 4
- Tiger 17
- Valproic Acid
- Valproic acid + PTD-DBM
- Vasoactive Intestinal Peptide
- Zinc-Thymulin
- Overall Health Benefits
- Key Takeaways
- What is Tranexamic Acid?
- Chemical Structure of Tranexamic Acid
- Research on Tranexamic Acid
- Tranexamic Acid Pills
- Tranexamic Acid Tablets
- Tranexamic Acid Uses
- Tranexamic Acid Side Effects
- Tranexamic Acid for Skin
- Tranexamic Acid Mechanism of Action
- Tranexamic Acid Dosage
- Tranexamic Acid Melasma
- Tranexamic Acid Topical
- Tranexamic Acid Mouthwash
- FAQ
- Reference
Table of Contents
- Overall Health Benefits
- Key Takeaways
- What is Tranexamic Acid?
- Chemical Structure of Tranexamic Acid
- Research on Tranexamic Acid
- Tranexamic Acid Pills
- Tranexamic Acid Tablets
- Tranexamic Acid Uses
- Tranexamic Acid Side Effects
- Tranexamic Acid for Skin
- Tranexamic Acid Mechanism of Action
- Tranexamic Acid Dosage
- Tranexamic Acid Melasma
- Tranexamic Acid Topical
- Tranexamic Acid Mouthwash
- FAQ
- Reference
Overall Health Benefits
- Brightens/Lightens the Skin [1-23]
- Treats Acne [24-31]
- Treats Rosacea [32-41]
- Treats Angioedema [42-60]
- Reduces Excessive Bleeding [61-74]
Key Takeaways
- Skin Lightening Agent: In skincare, it’s used to reduce hyperpigmentation, melasma, and post-inflammatory hyperpigmentation by inhibiting melanin production.
- Safe for Most Skin Types: It’s generally well-tolerated and suitable for various skin types. However, as with any skincare product, it’s advisable to consult with a dermatologist, especially if you have sensitive skin or underlying skin conditions.
- Effective When Combined with Other Ingredients: Tranexamic acid can work synergistically with other skincare ingredients like vitamin C and retinol to enhance its efficacy in brightening the skin.
- Gradual Results: While it’s a potent ingredient, results may take several weeks or even months to become noticeable. Patience and consistent use are key.
- Blood Clotting Agent: Its primary medical use is to prevent excessive bleeding, especially during surgeries and in cases of heavy menstrual bleeding.
What is Tranexamic Acid?
Tranexamic acid is a medication primarily used to reduce or prevent excessive bleeding. It works by inhibiting fibrinolysis, a process where blood clots are broken down in the body. By stabilizing these clots, tranexamic acid is effective in conditions like heavy menstrual bleeding, nosebleeds, and during surgeries to minimize blood loss.
Beyond its use for bleeding disorders, tranexamic acid has gained popularity in dermatology for its ability to treat hyperpigmentation. It inhibits melanin production, helping to fade dark spots and conditions like melasma when applied topically or taken orally. This dual-purpose medication is versatile in addressing both medical and cosmetic concerns.
While generally safe, tranexamic acid is not suitable for everyone. People with a history of blood clots, stroke, or certain kidney issues should avoid it. Side effects may include nausea, headaches, or stomach discomfort, and it’s essential to use it under medical supervision to ensure safe and effective outcomes.
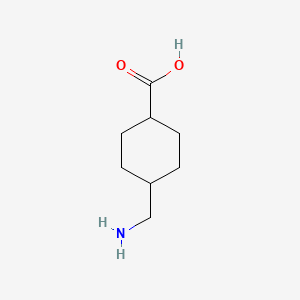
Chemical Structure of Tranexamic Acid
Tranexamic acid (TXA) is a synthetic derivative of lysine, an amino acid, with the chemical formula C8H15NO2. Its structure consists of a cyclohexane ring attached to an amino group (-NH2) and a carboxylic acid group (-COOH). This unique configuration gives it the ability to mimic lysine and bind to the lysine-binding sites on plasminogen, a precursor of plasmin, which plays a critical role in breaking down blood clots.
The cyclic nature of the cyclohexane ring in tranexamic acid provides rigidity to its structure, making it more effective at competitively inhibiting the activation of plasminogen compared to lysine itself. By preventing plasminogen from converting into plasmin, tranexamic acid stabilizes fibrin clots, thereby reducing excessive bleeding. This chemical mechanism underpins its use in both medical and cosmetic applications.
The molecular structure of tranexamic acid is both hydrophilic and lipophilic, allowing it to interact with biological membranes and proteins effectively. Its stable structure contributes to its high bioavailability and efficacy in various formulations, such as oral tablets, topical creams, and injections. These chemical properties are key to its versatility in treating conditions like hyperpigmentation, heavy menstrual bleeding, and surgical bleeding.
Research on Tranexamic Acid
A. Brightens/Lightens the Skin

Tranexamic acid brightens and lightens the skin by inhibiting melanin production. It blocks the interaction between keratinocytes and melanocytes by reducing the release of plasminogen activator, which decreases inflammation and UV-induced pigmentation. This action helps to fade hyperpigmentation conditions like melasma and improves overall skin tone.
- Melasma is a common hyperpigmentation disorder, particularly in individuals with skin of color, and tranexamic acid (TXA) has emerged as an effective treatment option. [1] Oral TXA, even at low doses (500 mg daily), has shown efficacy in improving melasma within 8–12 weeks, with a favorable safety profile and minimal side effects. It is recommended for refractory cases unresponsive to topical treatments, provided patients are screened for contraindications and thromboembolic risk factors.
- Tranexamic acid (TA) has been found to be an effective and safe topical treatment for melasma, comparable to the traditional combination of hydroquinone and dexamethasone. [2] In a 12-week split-face trial involving 50 Iranian women, both treatments significantly reduced melasma severity with similar patient and dermatologist satisfaction. However, TA had fewer side effects, making it a preferable option for managing melasma.
- Tranexamic acid, a synthetic derivative of lysine, is primarily used to reduce bleeding in surgical, trauma, and dental settings. [3] Its anti-inflammatory and melanin-suppressing properties make it effective in treating dermatological conditions like melasma, acne, post-inflammatory hyperpigmentation, and rosacea through oral, topical, or injectable routes. This review highlights its versatility and efficacy in managing various skin disorders.
- A study evaluated the effectiveness of low-dose oral tranexamic acid (250 mg twice daily) as an adjunct therapy for refractory melasma in 25 patients. [4] Results showed a significant 69% improvement in melasma severity, with mean MASI scores decreasing from 8.8 to 2.7 after 3.7 months of treatment (P < 0.01). The findings suggest oral tranexamic acid is a safe and effective option for managing melasma unresponsive to topical treatments.
- A randomized controlled trial compared the effectiveness of tranexamic acid (TA) combination serums (2% and 3%) with 4% hydroquinone for skin depigmentation. [5] Over 4 weeks, all groups showed significant improvements in skin brightness and pigmentation intensity, with no significant differences between the TA serums and hydroquinone. The study concluded that TA serums combined with galactomyces ferment filtrate, niacinamide, and alpha arbutin are effective depigmenting agents.
- Tranexamic acid (TXA) has been shown to reduce melanin synthesis in melanoma B16-F1 cells by activating the autophagy system and the ERK signaling pathway [6]. The study demonstrated that TXA enhances autophagy-related protein production while downregulating melanogenesis-associated proteins, including tyrosinase and MITF, leading to decreased melanin production. These findings suggest TXA’s potential as a mechanism-based skin-whitening agent.
- A study evaluated a gel serum containing tranexamic acid, niacinamide, 4-butylresorcinol, phytic acid, and hydroxy acids for its ability to reduce hyperpigmentation by targeting melanogenesis. [7] Results showed significant reductions in melanin production and brown spots within 14 days, with improvements sustained throughout treatment and maintained one month after cessation. The product demonstrated excellent skin tolerability, making it an effective and safe option for managing hyperpigmentation.
- A study compared the skin-lightening effects of oral and topical tranexamic acid (TXA) in a UVB-induced hyperpigmentation mouse model and human skin samples. [8] The results indicate that oral TXA is more effective than topical TXA in reducing hyperpigmentation by suppressing endothelin-1 (ET-1) production in vascular endothelial cells, which decreases melanogenesis and melanocyte proliferation. These findings highlight the superior efficacy of oral TXA in skin lightening through its impact on dermal microvascular pathways.
- Tranexamic acid, a plasmin inhibitor, is used off-label in dermatology for treating conditions like melasma, rosacea, and post-inflammatory hyperpigmentation due to its anti-inflammatory and anti-melanin properties. [9] While it shows promise for broader applications, caution is advised during the COVID-19 pandemic due to its procoagulant effects. Further studies are needed to explore its full potential in dermatology.
- Facial hyperpigmentation, a condition caused by excess melanin production, affects quality of life and self-esteem. [10] A study on 22 patients aged 45–67 tested a cream and serum containing tranexamic acid, niacinamide, vitamin C, and hyaluronic acid over 8 weeks. Results showed significant improvements in dark spot size and intensity, increased skin luminosity, and high user satisfaction, with minimal adverse effects. This combination offers a safe and effective alternative for managing hyperpigmentation and improving skin tone.
- A study evaluated a topical formulation containing tranexamic acid, niacinamide, and licorice for its efficacy in lightening facial pigmentation. [11] Among 50 female participants, 48 completed the study without tolerability issues, showing significant improvements in pigment intensity, extent, homogeneity, brightness, and clarity by Week 16. The results demonstrated the formulation’s effectiveness in reducing facial dyspigmentation safely and effectively.
- A study evaluated the efficacy and safety of topical tranexamic acid (TA) compared to a combination of hydroquinone and dexamethasone in treating melasma in Iranian women. Both treatments significantly reduced the Melasma Area and Severity Index (MASI) scores with similar satisfaction levels, but TA had fewer side effects. [12] The findings suggest TA is a safe and effective alternative for melasma treatment.
- Japanese pharmaceutical cosmetics, or quasi-drugs, use active ingredients like arbutin and rucinol to prevent pigmentation by suppressing melanin production, while others like disodium adenosine monophosphate reduce melanin accumulation. [13] Oral products containing vitamin C and tranexamic acid are more effective for treating freckles and melasma compared to quasi-drugs. This review categorizes skin-lightening ingredients by effectiveness and side effects, highlighting Japan’s advancements in this field.
- A study evaluated the safety and efficacy of a formula (TEST) containing astaxanthin, nicotinamide, arbutin, and tranexamic acid. [14] Results showed that TEST was safe, improved skin tone, and reduced melanin levels, suggesting its potential use in skin-whitening and spot-fading products.
- Oral tranexamic acid (TA) was studied as a treatment for melasma in 74 Chinese patients, with a dosage of 250 mg twice daily over six months. [15] Results showed improvement in pigmentation and melasma size, with 64.8% rated as excellent or good, though mild side effects like gastrointestinal discomfort and hypomenorrhea were noted. The study concluded that TA is a safe and effective therapy for melasma, with minimal recurrence observed.
- A study evaluated the effectiveness of a topical serum containing 3% tranexamic acid, 1% kojic acid, and 5% niacinamide in treating melasma, post-inflammatory hyperpigmentation (PIH), and hyperpigmentation over 12 weeks in Brazilian women. [16] Results showed significant improvements in pigmentation, skin tone, and texture starting at week 2, with continued progress through week 12, as confirmed by clinical assessments and melanin measurements. The serum was found to be an effective and well-tolerated treatment option for hyperpigmentary conditions, potentially acting by inhibiting inflammatory mediators involved in melanogenesis.
- Systemic therapies for skin lightening, such as oral carotenoids, glutathione, melatonin, and tranexamic acid, show promise in treating hyperpigmentation conditions like melasma and post-inflammatory hyperpigmentation. [17] While these treatments are generally safe, intravenous glutathione is discouraged due to potential adverse effects. Dermatologists must understand the efficacy and safety profiles of these therapies to counsel patients effectively on treatment expectations and proper use.
- A review explored the effectiveness of oral therapies, such as tranexamic acid, glutathione, isotretinoin, and proanthocyanidin, in treating various types of skin hyperpigmentation. [18] While these treatments show promise, their efficacy depends on addressing underlying causes like hormonal imbalances or metabolic conditions, and results for idiopathic cases are less predictable. Limitations include small sample sizes, lack of blinding, and a need for further research to confirm safety and effectiveness.
- A study evaluated the safety and efficacy of SKNB19, a non-hydroquinone (HQ) topical formulation, in treating hyperpigmentation compared to hydroquinone 4% (HQ4%). [19] Results showed SKNB19 significantly improved hyperpigmentation appearance by 28.5% (self-assessment) and 27% (independent assessment) over HQ4% while causing fewer adverse effects and being better tolerated. These findings suggest SKNB19 is a safe and effective alternative to HQ for managing hyperpigmentation.
- A study compared the efficacy and safety of transdermal injections of tranexamic acid (TA) and vitamin C (VC) in treating melasma. [20] Both treatments showed a significant reduction in MASI scores, with no statistically significant difference between the two. The treatments were well tolerated, with no serious side effects, suggesting that weekly TA or VC injections can be effective for melasma, although further research is needed.
- Topical tranexamic acid (TXA) is effective in treating melasma and skin hyperpigmentation caused by sunburn or inflammation. [21] It works by suppressing cytokine production, which reduces melanin synthesis and prevents excessive pigmentation. Studies suggest that TXA’s action involves inhibiting the plasminogen system in the epidermis and dermis, contributing to skin-lightening without forming thrombi in the vascular system.
- A pilot study evaluated the effectiveness of a topical combination of 2% tranexamic acid (TA) and 2% vitamin C in treating resistant melasma in 10 women from the Mediterranean region. [22] The results showed significant improvements in melasma severity, with the Melasma Area and Severity Index (MASI) score decreasing from 12.76 at baseline to 3.39 by Week 8. The treatment also led to a reduction in the Melasma Quality of Life Scale (MelasQoL) score and no major side effects were reported, suggesting this combination could be a safe and effective alternative to harsher treatments for melasma.
- A facial serum containing 2.0% cetyl tranexamate mesylate was tested for its safety and skin-lightening effects in a study with 54 participants. [23] The results showed significant improvements in melanin and erythema indexes, with subjects reporting better skin tone, reduced dark spots, and less facial redness after 2 weeks of use. The serum was well-tolerated, with no adverse reactions observed, making it an effective option for improving skin appearance and treating pigmentation issues.
B. Treats Acne

Tranexamic acid treats acne primarily by reducing inflammation and inhibiting the formation of blood clots, which can help in the healing process of acne lesions. It works by blocking the activation of plasminogen, reducing the release of pro-inflammatory substances that contribute to acne. This can help control breakouts, especially in individuals with inflammatory acne or those prone to post-inflammatory hyperpigmentation.
- A study evaluated the efficacy of 10% tranexamic acid (TXA) serum in treating mild-to-moderate acne, finding significant reductions in inflammatory acne, particularly papules and pustules, after 8 weeks of use. [24] TXA also decreased skin redness and post-inflammatory erythema (PIE) and hyperpigmentation (PIH), with minimal and treatable side effects. The results suggest that topical 10% TXA is an effective treatment for inflammatory acne with minor adverse effects.
- Topical 5% tranexamic acid (TXA) is an effective, well-tolerated treatment for reducing postinflammatory erythema (PIE) when applied nightly, with visible improvements within 6–8 weeks. [25] Its ease of use, lack of significant side effects, and ability to address skin redness make it a promising option for managing PIE and other erythema-related conditions.
- A study compared the efficacy of 20% azelaic acid (AZA) cream and 5% tranexamic acid (TA) solution for treating acne-related postinflammatory hyperpigmentation (PIH). [26] Both treatments showed similar improvements in the postacne hyperpigmentation index (PAHI) scores over 12 weeks, with no significant difference between the groups. However, TA had a better safety profile, with fewer side effects reported, particularly in the first month of treatment.
- Post-inflammatory hyperpigmentation (PIH) is a common complication after dermatologic procedures like laser treatments and chemical peels, and it can also result from conditions such as acne and burns. [27] High-risk patients, including those with Fitzpatrick skin types 3–5 or a history of PIH, are more likely to develop this condition. Tranexamic acid (TXA), an antifibrinolytic medication, has been used off-label to successfully treat and prevent PIH in high-risk patients, including those undergoing procedures like microneedling, cryotherapy, and chemical peels, with TXA being administered prophylactically in many cases.
- A study compared the efficacy of low-power fractional CO2 laser and tranexamic acid (TXA) microinjection for treating post-acne hyperpigmentation in patients resistant to regular treatments. [28] Both treatments showed significant improvement in pigmentation, but fractional CO2 laser demonstrated better results, particularly in dermoscopic scores. The study concluded that both methods are effective and safe, with fractional CO2 laser potentially offering superior results for post-acne hyperpigmentation.
- A study evaluated the efficacy of tranexamic acid (TA) mesotherapy for treating post-acne erythema (PAE) in 17 patients. [29] Results showed significant improvement in lesion count, area, and area percent on the treated side, with no notable changes on the control side. While TA injections appear effective for PAE, further research with larger sample sizes is needed to confirm these findings.
- Tranexamic acid, a synthetic derivative of lysine, is primarily used to reduce bleeding in medical and dental procedures but has found applications in dermatology for conditions like melasma, acne, and rosacea due to its anti-inflammatory and melanogenesis-suppressing properties. [30] It can be administered orally, topically, or via intradermal injection, often in combination with other treatments. This review highlights evidence supporting its effectiveness in treating various skin disorders.
- Tranexamic acid (TXA), a synthetic antifibrinolytic agent, is widely used for controlling bleeding in trauma, surgeries, and hemophilia. [31] Beyond its hemostatic applications, TXA has shown potential in treating hyperpigmentation and telangiectatic disorders through anti-inflammatory and skin barrier-repair effects, with oral, topical, and injectable modes of administration. While most research focuses on melasma, emerging evidence supports its use in conditions like post-inflammatory hyperpigmentation, rosacea, and post-acne erythema, offering safer and cost-effective treatment options.
C. Treats Rosacea

Tranexamic acid helps treat rosacea by reducing skin redness and inflammation. It works by inhibiting the breakdown of fibrin in the blood vessels, which can reduce the tendency for blood vessels to dilate and cause flushing or redness. This action helps improve the appearance of skin affected by rosacea, especially when used topically or as an oral treatment.
- Rosacea is a chronic inflammatory skin condition affecting the midface, characterized by erythema, flushing, and other symptoms. [32] While the precise pathophysiology remains unclear, tranexamic acid (TA), known for treating melasma and other skin conditions, has shown promise in alleviating rosacea symptoms through mechanisms like barrier restoration and angiogenesis inhibition. This review explores the therapeutic potential of TA for rosacea via various delivery methods, including oral, topical, and advanced techniques like microneedling and laser-assisted delivery.
- Tranexamic acid (TXA) has shown promising results in treating papulopustular rosacea (PPR) by enhancing skin barrier function, reducing dryness, and improving overall skin hydration. [33] A study involving 70 patients demonstrated that adding oral TXA to traditional therapy significantly improved clinical outcomes, patient satisfaction, and quality of life compared to traditional therapy alone, with better results observed in dry-type rosacea. TXA was well-tolerated, with no significant side effects reported.
- Tranexamic acid (TXA) has emerged as an effective treatment for rosacea by regulating immune responses and angiogenesis. [34] In LL37-induced mouse and HaCaT cell models, TXA reduced skin erythema, pro-inflammatory cytokines (IL-6, TNFα), and angiogenesis markers like VEGF, while modulating both innate and adaptive immune responses. These findings highlight TXA’s therapeutic potential in mitigating inflammation and vascular hyperreactivity in rosacea.
- A study evaluated the efficacy of topical tranexamic acid for treating erythematotelangiectatic rosacea in 20 women aged 27–65 years. [35] Patients treated with tranexamic acid alone or combined with microneedling showed significant improvement, with better outcomes in the combined treatment group. The therapy was well-tolerated, effective, and offers a promising, safe, and cost-effective option for managing rosacea symptoms.
- A study evaluated the efficacy of 10% topical tranexamic acid (TXA) with and without microneedling for treating erythematotelangiectatic rosacea (ETR). [36] Both treatments showed improvement, but combining TXA with microneedling resulted in significantly better outcomes for reducing erythema and telangiectasia. The study concludes that TXA is effective and safe, with microneedling enhancing its delivery and efficacy.
- Intradermal microinjections of tranexamic acid (TXA) were evaluated as a treatment for erythematotelangiectatic rosacea (ETR) in a retrospective study of six patients. [37] Results showed a significant reduction in rosacea severity scores, with transient local side effects but no systemic effects. TXA microinjections appear to be a safe and effective option for ETR, though the optimal treatment schedule requires further study.
- A study published in Archives of Dermatological Research evaluated the clinical efficacy and impact on quality of life of tranexamic acid (TXA) in patients with rosacea. [38] The findings suggest that TXA treatment may offer benefits for rosacea management.
- Topical application of 10% tranexamic acid (TXA) has been found to significantly reduce erythema, telangiectasia, and burning sensations associated with steroid-induced rosacea within 4 to 6 weeks of treatment. [39] This approach is noted for its ease of preparation and favorable tolerability profile.
- A novel topical application of tranexamic acid (TA) using TA-loaded ZIF-8 (TA@ZIF-8) enhances its penetration through the skin barrier and addresses limitations of systemic use and traditional transdermal delivery methods. [40] TA@ZIF-8 improves drug encapsulation, intracellular uptake, and activates the aquaporin-3 protein, resulting in effective treatment of melasma and rosacea with minimal cytotoxicity. Clinical trials confirm its safety and efficacy, presenting a promising alternative to systemic administration for anti-inflammatory and anti-pigmentation therapies.
- A study evaluated the efficacy and safety of a topical triple combination (tranexamic acid 5%, oxymetazoline 1.5%, and brimonidine tartrate 0.33%) for treating persistent post-acne erythema (PAE) in a split-face study involving 40 patients over three months. [41] Results showed that the combination treatment significantly reduced PAE on the treated side compared to the placebo, confirming it as a safe and cost-effective option. The findings highlight its potential as an innovative therapy for addressing PAE.
D. Treats Angioedema

Tranexamic acid treats angioedema by inhibiting the activation of plasminogen to plasmin, which reduces the breakdown of fibrin and decreases the release of inflammatory mediators involved in swelling. This helps prevent or reduce the severity of episodes by stabilizing the blood vessels and reducing fluid leakage into surrounding tissues.
- Hereditary angioedema (HAE) is a life-threatening inherited condition characterized by swelling attacks, often starting in childhood, that are unresponsive to standard allergy treatments. [42] While effective treatments exist for adults, options for children under 12 are limited, with only one approved medication. The Medical Advisory Board, in collaboration with the HAE Patient’s Association, has developed consensus recommendations to guide the recognition, diagnosis, and treatment of HAE in children.
- Hereditary angioedema (HAE) is a rare, life-threatening condition caused by C1 esterase inhibitor deficiency, leading to swelling in the skin, gastrointestinal, and respiratory tracts.[43] This case highlights a pregnant woman with worsening HAE, managed effectively with danazol, tranexamic acid, and regular intravenous C1 esterase inhibitor therapy.
- Tranexamic acid (AMCA) effectively managed hereditary angioneurotic edema in six out of seven Finnish patients, with some achieving near symptom-free status on continuous treatment. However, one patient discontinued AMCA due to fatigue and nausea. [44] In comparison, antihistamine treatment with cinnarizine also helped two out of three patients by reducing attack frequency and severity.
- Tranexamic acid (TA) appears to be an effective and well-tolerated maintenance treatment for some patients with hereditary angioedema (HAE) or idiopathic non-histaminergic angioedema (AE), reducing attack frequency by 75% in nearly half of the patients studied over six months. [45] The study, involving 37 cases, reported no increase in symptoms or thromboembolic events, with digestive side effects being the most common. TA offers a promising, affordable option for managing non-histaminergic AE.
- Long-term prophylaxis for hereditary angioedema presents challenges due to side effects of current treatments. [46] While attenuated androgens are effective, tranexamic acid and progestagens offer alternatives with fewer side effects, particularly for children and women. C1 inhibitor therapy is effective but requires intravenous administration, and new therapies show promise in addressing current limitations.
- A study evaluated treatments for hereditary angioedema in 20 patients, focusing on the effectiveness of tranexamic acid and intravenous infusions of kallikrein inhibitor or C1 esterase inhibitor concentrate. [47] Tranexamic acid prevented swellings in most cases without serious side effects, while C1 esterase inhibitor concentrate was highly effective for acute attacks, showing faster improvement compared to kallikrein inhibitor. Serum levels of C4 and C1 esterase inhibitor were also assessed before and after treatments.
- In Peru, Tranexamic Acid (TA) has been used successfully in managing hereditary angioedema (HAE) in patients for both prophylactic and acute treatment. [48] Case studies of three women with different HAE subtypes demonstrated that TA, administered in varying oral and intravenous doses, effectively reduced symptoms and controlled acute crises, especially where specific HAE treatments were unavailable. High doses of TA were well-tolerated and showed acceptable responses, suggesting its potential as an alternative treatment in regions without registered HAE-specific therapies.
- C1-inhibitor deficiency causes mucocutaneous edema and may be hereditary or acquired, with the acquired form (AAE) responding better to antifibrinolytic agents like tranexamic acid. [49] A study of eight patients with autoimmune AAE showed elevated levels of cleaved high molecular weight kininogen and antiplasmin-plasmin complexes in all conditions, along with inactive C1-inhibitor. Prophylactic treatment reduced symptoms but did not significantly alter these biochemical markers.
- Tranexamic acid (TA) has shown promise as a maintenance treatment for non-histaminergic angioedema (AE), including hereditary AE and idiopathic non-histaminergic AE, according to a national retrospective study. [50] Over six months, TA reduced attacks by 75% in nearly half of the patients, with no increase in symptoms or thromboembolic events. TA is well-tolerated, cost-effective, and may benefit select AE patients, though digestive side effects were noted.
- Tranexamic acid (TXA) is an antifibrinolytic agent primarily used to manage hereditary angioedema by inhibiting plasminogen activation and bradykinin formation. [51] Although evidence is limited, a case report suggests TXA may also be effective in treating ACE inhibitor-induced angioedema (ACEI-AE), highlighting its potential as a treatment option and the need for further research.
- A study evaluated the use of tranexamic acid (TXA) in managing angiotensin-converting enzyme inhibitor-induced angioedema (ACEi-AE) in the emergency department (ED). [52] Of the 16 patients treated, only 2 required intubation before TXA administration, and none needed intubation afterward, suggesting TXA may be effective in reducing intubation rates. TXA was also associated with a low rate of adverse effects, making it a promising addition to standard care for ACEi-AE.
- Hereditary angioedema is a genetic condition causing recurrent swelling of the extremities, face, airway, or abdomen, often triggered spontaneously or by trauma. [53] Diagnosis involves detecting low C4 or C1 esterase inhibitor activity, and treatment includes long-term and short-term prophylaxis with antifibrinolytic agents, androgens, or plasma transfusions, as well as supportive care during acute attacks to prevent complications like airway obstruction. Advances in therapy have significantly reduced mortality rates, which were historically as high as 30%.
- C1 Inhibitor deficiency causes uncontrolled complement activation, leading to unpredictable and potentially life-threatening angioedema. [54] While plasma-derived C1 Inhibitor can rapidly treat attacks, it is costly and may not work in cases of autoantibody-mediated angioedema. Antifibrinolytic agents like tranexamic acid are effective for prophylaxis, and novel treatments such as the kallikrein inhibitor DX-88 are under clinical investigation.
- Hereditary angioedema (HAE) is a nonhistamine-mediated condition causing tissue edema that does not respond to standard treatments like epinephrine or antihistamines. [55] It is managed with therapies such as tranexamic acid, C1 esterase inhibitors, or fresh-frozen plasma, and airway intervention may be needed in acute cases. Minor trauma or stress can trigger delayed swelling, and angiotensin-converting enzyme inhibitors may worsen symptoms.
- Hereditary angioedema (C1-INH-HAE) is a rare genetic disorder that has seen significant advancements in treatment over the past decade, particularly through targeting the kallikrein-kinin system. [56] Current therapies focus on acute treatment, short-term prophylaxis, and long-term prophylaxis, with several drugs approved for self-administration. Ongoing research is exploring new drugs aimed at blocking the kallikrein-kinin system to improve long-term management of C1-INH-HAE.
- A study evaluated three familial generations with hereditary angioneurotic edema (HAE), focusing on clinical and immunological factors. [57] The trial with tranexamic acid demonstrated its effectiveness in treating HAE, showing fewer side effects compared to other treatments. The study also highlighted the importance of screening asymptomatic family members to detect low plasma levels of C1-INH.
- Acquired angioedema (AAE) is a rare condition often linked to lymphoproliferative disorders and anti-C1 esterase inhibitor antibodies, with no standardized treatment. [58] A retrospective review of 13 patients showed that tranexamic acid (TXA) significantly reduced AAE attacks by up to 99% over 24 months, making it an effective prophylactic option. However, adverse effects, such as a deep vein thrombosis in one patient, highlight the need for further treatment alternatives.
- A double-blind study treated 10 patients with non-hereditary angioedema using tranexamic acid or placebo for 3 months. [59] Nine patients showed significant improvement with tranexamic acid, while one was unaffected, and side effects like diarrhea and abdominal discomfort occurred in some cases. Four years later, six responders were still using tranexamic acid regularly, with two using it less frequently due to reduced attacks.
- In a double-blind study of 10 patients with non-hereditary angioedema, 9 showed significant improvement or became symptom-free with tranexamic acid treatment compared to placebo (P < 0.05), while itching improved in 3 of 4 affected patients. [60] Although diarrhea and abdominal discomfort were more frequent (P < 0.05), only one required a dose reduction. Four years later, 6 of 8 responders continued regular use, while 2 reported infrequent attacks and no longer required consistent treatment.
E. Reduces Excessive Bleeding
Tranexamic acid reduces excessive bleeding by inhibiting the activation of plasminogen to plasmin, a protein that breaks down fibrin in blood clots. By blocking this process, tranexamic acid helps stabilize the clot and prevents further breakdown, thereby promoting clot retention and reducing bleeding, especially in conditions like heavy menstrual bleeding, trauma, or surgery.
- Tranexamic acid (TXA) reduces blood loss by preventing fibrin breakdown and is widely used in surgery and trauma care to decrease bleeding and the need for transfusion. [61] The CRASH-2 trial demonstrated that TXA, administered within 3 hours of injury, reduces the risk of death from hemorrhage by about one-third without significant adverse effects, making it suitable for a broad range of bleeding trauma patients. Restricting its use could lead to preventable deaths, and ongoing research, such as the CRASH-3 trial, is exploring its potential benefits in traumatic brain injury.
- Uncontrolled massive bleeding, often caused by hyperfibrinolysis (HF), poses a significant challenge in managing surgical and trauma patients, especially those involving organs rich in plasminogen activators. [62] HF leads to excessive bleeding and high mortality, requiring effective intervention. Tranexamic acid (TXA), a synthetic lysine analogue available since 1966, is a crucial antifibrinolytic for preventing and treating HF-related bleeding, reducing perioperative blood loss and transfusion needs. Its applications span various hemorrhagic conditions, with guidelines and research supporting its indications and dosages.
- Tranexamic acid (TXA), an antifibrinolytic agent originally developed for postpartum hemorrhage (PPH), has shown efficacy in managing active bleeding across various clinical contexts, with effectiveness influenced by timing, dose, and setting. [63] Early administration is crucial, particularly in trauma and PPH, and while TXA generally does not increase thrombotic risks, it may raise venous thrombosis risk in gastrointestinal bleeding and seizure risk at higher doses. Further research is needed to optimize dosing, administration, and understand its mechanisms in contexts like intracerebral hemorrhage, emphasizing individualized patient assessment and context-specific evidence to improve outcomes.
- The HALT-IT trial found no evidence that tranexamic acid (TXA) reduces mortality in gastrointestinal bleeding, but a systematic review and meta-analysis of 64,724 patients across four large trials showed TXA reduces the odds of death by 16% overall and by 20% when administered within 3 hours of bleeding onset, without increasing vascular occlusive events. [64] These findings suggest that the HALT-IT results align with evidence supporting TXA’s efficacy in reducing mortality across various bleeding conditions.
- Tranexamic acid has gained significant attention for its ability to reduce morbidity and mortality in surgical and traumatic bleeding. [65] It reduces traumatic bleeding mortality by a third and minimizes blood loss and transfusion needs in surgical patients, with both intravenous and topical applications. While generally safe, high doses may cause neurological side effects without added efficacy, as studies show 1 g intravenously is optimal. The CRASH-2 trial demonstrated no increased thrombotic risk and even reduced myocardial infarction rates, though further research is needed to assess its effects on postoperative venous and arterial thromboembolism in surgical settings.
- Tranexamic acid is a safe and effective treatment for heavy menstrual bleeding and postpartum hemorrhage, significantly improving quality of life, reducing mortality risk, and enabling better participation in daily activities. [66] However, its widespread use is hindered by barriers such as structural sexism, period poverty, stigmatization of vaginal blood loss, misinformation in labeling, and limited drug access, which perpetuate inequities in women’s health. The evidence supporting its benefits and the challenges to its utilization were highlighted at the 2023 International Society on Thrombosis and Haemostasis Congress.
- A systematic review and meta-analysis of 129 randomized controlled trials involving 10,488 patients found that tranexamic acid significantly reduces the need for blood transfusions in surgical patients by approximately one-third, with strong evidence supporting its efficacy. [67] However, its impact on thromboembolic events (e.g., myocardial infarction, stroke, deep vein thrombosis, and pulmonary embolism) and mortality remains uncertain. While fewer deaths were observed in the tranexamic acid group, the evidence was less robust when restricted to trials with adequate allocation concealment. Further research on its effects on thromboembolic events and mortality is needed, and patients should be informed of these findings to make informed decisions.
- Early use of tranexamic acid significantly reduces postpartum hemorrhage (PPH) deaths, with major implications for global obstetrical care, particularly in low- and middle-income countries where access is limited. [68] Beyond PPH, tranexamic acid could address maternal anemia by reducing heavy menstrual bleeding, improve blood availability by minimizing surgical blood loss, and lower healthcare costs by reducing transfusions and associated risks. Expanding its use in trauma care could also reduce mortality from violence and injuries. Collaborative efforts to increase access should highlight these broader health benefits to promote its integration across diverse healthcare settings.
- Tranexamic acid (TXA) effectively reduces bleeding in various clinical settings, including surgeries, trauma, and certain bleeding disorders, with strong evidence for its use in menorrhagia, postpartum hemorrhage, and trauma-related mortality reduction. [69] While generally safe, high doses can increase seizure risk in brain injury and cardiac surgery, and delayed administration in trauma or postpartum hemorrhage may raise mortality. Evidence for efficacy in traumatic brain injury and gastrointestinal bleeding is lacking, and thrombotic risks remain a concern in specific scenarios. Ongoing research aims to refine TXA’s optimal dosing and timing to balance its benefits and risks.
- In patients with advanced liver cirrhosis (Child-Turcotte-Pugh class B or C) presenting with upper gastrointestinal bleeding (UGIB), tranexamic acid significantly reduced the failure to control bleeding by day 5 (6.3% vs. 13.3%, p=0.006) and failure to prevent rebleeding from esophageal variceal ligation (EVL) sites compared to placebo, though mortality rates at 5 days and 6 weeks were similar between groups. [70]
- This systematic review and meta-analysis of 13 randomized controlled trials (n=2271) demonstrates that tranexamic acid significantly reduces continued bleeding, urgent endoscopic intervention, and mortality in patients with upper gastrointestinal bleeding, supporting its use in emergency settings. [71] However, its effects on lower gastrointestinal bleeding remain unclear and require further investigation.
- Tranexamic acid, a synthetic lysine derivative, effectively reduces blood loss and transfusion needs in various surgeries, including cardiac, oral, and liver procedures, and shows efficacy in treating upper gastrointestinal bleeding, menorrhagia, and pregnancy-related bleeding. [72] It demonstrates comparable or superior benefits to other antifibrinolytics, such as aprotinin, with a favorable safety profile and no increased thrombosis risk in clinical trials.
- The study evaluated the efficacy and safety of tranexamic acid (TXA) in gastrointestinal bleeding through a systematic review and meta-analysis of randomized controlled trials. [73] Extended-use high-dose IV TXA did not reduce mortality or bleeding and was associated with an increased risk of adverse events, including deep venous thrombosis, pulmonary embolism, and seizures. In contrast, low-dose IV or enteral TXA showed moderate evidence of reducing rebleeding and the need for surgery without improving mortality, highlighting the need for further research to confirm its safety and efficacy.
- This double-blind, placebo-controlled study demonstrated that oral tranexamic acid (3.9 g/day) significantly reduced menstrual blood loss and improved health-related quality of life in women with heavy menstrual bleeding. [74] Over six cycles, tranexamic acid achieved a 40.4% reduction in menstrual blood loss compared to 8.2% with placebo, meeting all primary efficacy endpoints. Women treated with tranexamic acid reported meaningful improvements in physical, social, and work activities, with most adverse events being mild to moderate and similar in frequency to placebo.Tranexamic acid (TXA) is a widely researched antifibrinolytic agent effective in managing bleeding from surgery, trauma, obstetric complications, and various hemostatic disorders. Its established roles in postpartum hemorrhage, menorrhagia, trauma-related bleeding, and surgical bleeding are complemented by emerging evidence of broader applications, demonstrating its ability to reduce bleeding and improve outcomes without significantly increasing thrombotic risk.
Tranexamic Acid Pills
Tranexamic acid pills are a medication primarily used to treat and prevent excessive bleeding. They work by inhibiting the breakdown of blood clots, helping to stabilize clot formation and reduce blood loss. These pills are often prescribed for conditions such as heavy menstrual bleeding, nosebleeds, or to manage bleeding after surgeries or dental procedures.
For those experiencing heavy menstrual bleeding, tranexamic acid pills can significantly reduce the volume of blood lost during periods. They are taken only during active bleeding, typically for a few days, making them a targeted and convenient solution. The medication is effective within hours of the first dose, providing timely relief for individuals with bleeding disorders.
Although generally well-tolerated, tranexamic acid pills may have side effects, including nausea, headache, or stomach discomfort. Certain individuals, such as those with a history of blood clots, kidney disease, or stroke, should avoid this medication. It is important to use tranexamic acid under medical supervision to ensure its safety and efficacy for specific health needs.
Tranexamic Acid Tablets
Tranexamic acid tablets are primarily used to control excessive bleeding in various medical conditions, such as heavy menstrual periods (menorrhagia), nosebleeds, or bleeding after surgeries and dental procedures. They work by inhibiting the breakdown of blood clots, helping to reduce blood loss effectively. This makes them an essential medication for individuals prone to bleeding disorders or situations requiring temporary clot stabilization.
The tablets are generally taken for short durations during periods of active bleeding. For menstrual bleeding, they are typically used for 3–5 days during the heaviest flow days. While tranexamic acid is highly effective, it’s important to take it under medical supervision, as it can increase the risk of blood clots in certain individuals, particularly those with a history of thromboembolic disorders or certain underlying health conditions.
Potential side effects of tranexamic acid tablets include nausea, headache, stomach upset, and, in rare cases, an increased risk of clotting. Patients should avoid combining it with other medications that elevate clotting risk, such as certain hormonal contraceptives, without consulting a doctor. Despite these considerations, when used appropriately, tranexamic acid tablets are a safe and effective solution for managing excessive bleeding.
Tranexamic Acid Uses
Tranexamic acid is widely used to treat and manage excessive bleeding in various medical conditions. It is commonly prescribed for heavy menstrual bleeding (menorrhagia), helping to reduce blood loss and make periods more manageable. Additionally, it is often used in surgical settings to prevent excessive bleeding during or after operations, especially in patients with a higher risk of bleeding disorders.
Beyond its role in managing bleeding, tranexamic acid is also effective in dermatology for treating skin hyperpigmentation conditions like melasma and dark spots. It works by inhibiting melanin production, which helps improve skin tone and reduce discoloration over time. Available in both oral and topical formulations, it provides a versatile option for addressing pigmentation concerns.
In dentistry, tranexamic acid is used to control bleeding following dental surgeries or in patients with bleeding disorders undergoing oral procedures. It may be used as a mouthwash or in other forms to stabilize clots and minimize post-procedure blood loss. These varied uses highlight its effectiveness in managing conditions involving excessive bleeding and pigmentation issues.
Tranexamic Acid Side Effects
Tranexamic acid is generally well-tolerated, but like any medication, it can cause side effects in some individuals. Common side effects include nausea, vomiting, diarrhea, and stomach pain, which are usually mild and temporary. Some people may also experience headaches or fatigue during treatment.
More serious side effects, though rare, can include blood clots, visual disturbances, and allergic reactions such as swelling or rash. These risks are higher in individuals with a history of blood clotting disorders or those taking medications that increase clotting risks. It’s essential to monitor for symptoms like chest pain, shortness of breath, or leg swelling and report them immediately to a healthcare provider.
In skincare formulations, tranexamic acid can occasionally cause irritation, redness, or sensitivity, especially when used in high concentrations or alongside other potent actives. To minimize these effects, patch testing and using products as directed can help ensure safe and effective use. Always consult a healthcare professional before starting tranexamic acid for any purpose.
Tranexamic Acid for Skin
Tranexamic acid is a powerful ingredient for addressing hyperpigmentation and uneven skin tone. It works by inhibiting the production of melanin, the pigment responsible for dark spots and discoloration. This makes it particularly effective for treating conditions like melasma, post-inflammatory hyperpigmentation, and sunspots. Unlike some harsh brightening agents, tranexamic acid is generally well-tolerated, even on sensitive skin.
Topical tranexamic acid is available in various formulations, such as serums and creams, and is often combined with other skin-brightening ingredients like niacinamide or vitamin C for enhanced results. When used consistently, it can visibly reduce dark spots within 4–8 weeks, helping to achieve a more even and radiant complexion. It’s a suitable option for those seeking a gentler alternative to hydroquinone.
To maximize the benefits of tranexamic acid for skin, it’s essential to pair it with sunscreen. Sun exposure can exacerbate pigmentation issues, and sunscreen helps protect the skin while allowing the acid to work effectively. Regular use, combined with a comprehensive skincare routine, can yield significant improvements in pigmentation and overall skin texture.
Tranexamic Acid Mechanism of Action
Tranexamic acid works by inhibiting the activation of plasminogen to plasmin, an enzyme responsible for breaking down fibrin clots. By blocking this process, tranexamic acid stabilizes the fibrin matrix within blood clots, preventing excessive bleeding and promoting clot preservation in areas where bleeding control is needed.
This mechanism makes tranexamic acid particularly effective in conditions involving hyperfibrinolysis, such as heavy menstrual bleeding, trauma-related hemorrhage, and post-surgical blood loss. By reducing the breakdown of clots, it minimizes blood loss without interfering with the natural clot formation process.
Tranexamic acid’s ability to stabilize clots also extends to its topical and cosmetic applications, such as reducing melanin-related pigmentation in the skin. In this context, it inhibits plasmin-induced inflammatory mediators in the skin, contributing to improved skin tone and reduced dark spots.
Tranexamic Acid Dosage
Tranexamic acid dosage depends on the condition being treated and the patient’s individual health factors. For heavy menstrual bleeding, the typical dosage is 1,000–1,500 mg taken orally two to three times daily during the first three to five days of the menstrual cycle. This helps significantly reduce blood loss while maintaining a manageable treatment duration.
In surgical or dental procedures, tranexamic acid is often administered intravenously or orally to prevent excessive bleeding. The dosage typically ranges from 10–15 mg per kilogram of body weight every eight hours, depending on the procedure and patient risk factors. For topical use in dentistry or dermatology, concentrations are lower and depend on the specific formulation prescribed.
It is important to follow the prescribed dosage exactly as directed, as excessive use of tranexamic acid can increase the risk of side effects such as nausea, headaches, or blood clots. Always consult a healthcare provider before starting or adjusting the dosage to ensure it is safe and effective for your specific needs.
Tranexamic Acid Melasma
Tranexamic acid has emerged as an effective treatment for melasma, a chronic skin condition characterized by dark patches on the face. It works by inhibiting the enzyme plasmin, which can trigger inflammatory pathways and melanin production in the skin. By targeting these processes, tranexamic acid reduces the pigmentation associated with melasma and improves overall skin tone.
Available in various forms, including oral tablets, topical creams, and injectables, tranexamic acid offers flexibility in treating melasma. Topical formulations are often preferred for mild cases due to their minimal side effects, while oral or injectable options may be recommended for more severe cases. Results typically become noticeable within 4–8 weeks of consistent use, though longer treatment durations may be needed for significant improvement.
Despite its benefits, tranexamic acid is not without potential side effects. Topical use can sometimes cause irritation or redness, while oral treatments carry a small risk of clotting issues. As such, it is essential to use tranexamic acid under medical supervision, particularly for those with a history of blood clotting disorders or other health concerns.
Tranexamic Acid Topical
Tranexamic acid topical is a skincare ingredient gaining popularity for its effectiveness in treating hyperpigmentation and melasma. It works by inhibiting the production of melanin, the pigment responsible for dark spots, making it an ideal choice for those looking to achieve a more even skin tone. This gentle yet effective treatment is suitable for various skin types and can be incorporated into a daily skincare routine.
One of the key advantages of tranexamic acid in topical formulations is its ability to reduce discoloration without causing significant irritation, unlike some stronger treatments such as hydroquinone. Regular application, typically over 4–8 weeks, can lead to visible improvements in the appearance of dark spots and an overall brighter complexion. It is often combined with other skin-brightening agents like niacinamide for enhanced results.
However, like all active ingredients, tranexamic acid should be used as directed to avoid overuse or potential irritation. Those with sensitive skin may want to start with a lower concentration and patch-test before widespread application. For the best outcomes, it is also essential to pair tranexamic acid with daily sunscreen use to prevent further pigmentation from UV exposure.
Tranexamic Acid Mouthwash
Tranexamic acid mouthwash is a specialized solution used to control and prevent bleeding in the oral cavity. It is commonly prescribed after dental procedures, such as tooth extractions, to minimize bleeding in patients with bleeding disorders or those taking anticoagulant medications. The active ingredient works by stabilizing blood clots and preventing their premature breakdown, ensuring effective hemostasis.
The mouthwash is typically prepared in a diluted concentration and used as a rinse multiple times a day, depending on the severity of bleeding and the dentist’s or doctor’s recommendation. It is particularly effective for individuals who cannot stop anticoagulant therapy, offering a safe way to manage bleeding without interfering with systemic medications.
While tranexamic acid mouthwash is generally safe, it may cause mild side effects such as a temporary metallic taste or irritation in some users. Patients should follow usage instructions carefully and inform their healthcare provider about any pre-existing conditions or medications to ensure its safe and effective use.
FAQ
What does tranexamic acid do to you?
Tranexamic acid helps reduce or stop bleeding by preventing the breakdown of blood clots. If a missed dose occurs, it’s important to take the medication as soon as you remember, unless it’s almost time for your next dose. Missing a dose of tranexamic acid can reduce its effectiveness in controlling bleeding, so it’s essential to follow the prescribed schedule carefully to avoid a missed dose and ensure optimal results.
What is tranexamic acid best for?
It is best for treating heavy menstrual bleeding, managing bleeding disorders, and preventing excessive blood loss during surgeries. If you have a history of blood clots or other related conditions, tell your doctor before using tranexamic acid. Additionally, if you experience any unusual symptoms while taking the medication, such as swelling or pain, tell your doctor to ensure safe use. Always follow your healthcare provider’s advice and tell your doctor if you are taking any other medications that might interact with tranexamic acid.
Who should not use tranexamic acid?
People with a history of blood clots, stroke, kidney disease, or hypersensitivity to the drug should not use tranexamic acid. Be sure to tell your doctor if you have any of these conditions before starting the medication. Additionally, tell your doctor about any other medications or supplements you are taking to avoid potential interactions. If you experience any unusual side effects, tell your doctor immediately.
How does tranexamic acid stop periods?
It reduces menstrual bleeding by stabilizing clots in the uterine lining, preventing further blood loss and minimizing the risk of allergic reactions. However, in rare cases, allergic reactions may occur, so monitoring for any signs is essential. Always consult a doctor if you suspect allergic reactions to this medication.
What do tranexamic acid pills do?
Tranexamic acid pills reduce excessive bleeding by slowing the breakdown of blood clots, making them a valuable option for those on birth control pills who experience heavy periods. When used alongside birth control pills, tranexamic acid can help manage abnormal menstrual bleeding more effectively. It’s important to consult a doctor before combining tranexamic acid pills with birth control pills to ensure safe and effective use.
Can you buy tranexamic over the counter?
In most countries, tranexamic acid requires a prescription, though in some regions, lower doses may be available over the counter for conditions such as deep vein thrombosis. It is essential to consult a healthcare provider before use, especially if there is a history of deep vein thrombosis or related clotting disorders. Monitoring is crucial when using medications like tranexamic acid to manage risks such as deep vein thrombosis effectively.
How long does tranexamic acid take to stop bleeding?
It can start working within 2–4 hours, with significant reduction in bleeding often observed within a day. If bleeding persists, you may need to take your next dose as directed by your healthcare provider. Be sure to follow the recommended timing for your next dose to ensure optimal effectiveness and avoid complications.
Who cannot take tranexamic acid?
See above: individuals with blood clotting disorders, strokes, or severe kidney issues should avoid tranexamic acid. Tranexamic acid is commonly prescribed to treat heavy bleeding, especially during menstruation or after surgery. However, people with certain medical conditions should consult a healthcare provider before using it to treat heavy bleeding, as it may pose risks for those with clotting issues.
What is tranexamic acid tablets used for?
They are used to treat heavy menstrual bleeding, nosebleeds, and to prevent excessive bleeding during surgeries or dental procedures, under the guidance of a healthcare professional. A healthcare professional can help determine the appropriate dosage and duration of tranexamic acid treatment based on individual needs. Always consult a healthcare professional before starting any treatment to ensure it is safe and effective for your specific condition.
How long does it take tranexamic acid to stop bleeding?
Typically, it starts reducing bleeding within a few hours, with maximum effect seen after consistent use for 1–2 days. If you experience any adverse reactions or side effects, you may need to stop taking tranexamic acid and consult your healthcare provider. In most cases, it’s safe to continue use as prescribed, but if you feel any unusual symptoms, it’s important to stop taking tranexamic acid and seek medical advice. Always follow the recommended dosage, and if in doubt, stop taking tranexamic acid and reach out to your doctor.
Can you buy tranexamic acid over the counter?
See above: availability depends on the country, but it generally requires a prescription. People with a history of pulmonary embolism should be cautious when considering medications like tranexamic acid. Always consult with a healthcare provider, especially if you have a condition like pulmonary embolism, to ensure safety before using any new treatment.
What are the side effects of tranexamic acid on your period?
Side effects may include nausea, stomach pain, headache, or changes in menstrual flow. If you experience any unusual symptoms, it’s important to consult an eye doctor, as some side effects could affect your vision. Additionally, if you have concerns about any ongoing symptoms, an eye doctor can provide specialized guidance.
What is the main use of tranexamic acid?
Its primary use is to control and prevent excessive bleeding, especially when followed under a regular dosing schedule. By adhering to a regular dosing schedule, tranexamic acid helps maintain steady levels in the body, ensuring its effectiveness in reducing blood loss. For optimal results, it is important to stick to a regular dosing schedule as prescribed by a healthcare professional.
What are the disadvantages of tranexamic acid?
Disadvantages include side effects like nausea, an increased risk of blood clots, and contraindications for certain medical conditions. Tranexamic acid is often used to treat heavy menstrual bleeding, and while it is effective, it can carry risks for individuals with a history of clotting disorders. Additionally, when used to treat heavy bleeding, it’s important to monitor for potential side effects and ensure it is appropriate for your condition.
What to avoid when taking tranexamic acid?
Avoid taking it with hormonal contraceptives or medications that increase clotting risk without consulting a doctor. If you miss a dose, skip the missed dose and take your next dose at the regular time. It’s important not to double the dose to make up for a missed dose; simply skip the missed dose and continue with your regular schedule. Always follow your doctor’s instructions and don’t skip the missed dose if you’re uncertain about how to proceed.
What to avoid when taking tranexamic acid?
Avoid taking it with hormonal contraceptives or medications that increase clotting risk without consulting a doctor. If you miss a dose, skip the missed dose and take your next dose at the regular time. It’s important not to double the dose to make up for a missed dose; simply skip the missed dose and continue with your regular schedule. Always follow your doctor’s instructions and don’t skip the missed dose if you’re uncertain about how to proceed.
What are the negative effects of tranexamic acid?
Potential negative effects include headaches, nausea, and an increased risk of blood clots, as noted on the prescription label. It’s important to follow the instructions on the prescription label carefully to avoid these side effects. If any adverse reactions occur, consult your healthcare provider and review the prescription label for any necessary adjustments to your dosage.
What happens to your period when you take tranexamic acid?
Periods typically become lighter and shorter when taking tranexamic acid, as it helps reduce excessive bleeding. However, some individuals may experience adverse effects, such as nausea or headaches, when using the medication. It’s important to monitor for any adverse effects and consult a healthcare provider if they persist or worsen.
How long can you safely take tranexamic acid?
It is usually taken for short durations during active bleeding, such as 3–5 days per cycle for menstrual bleeding, but it’s important to check for interactions with other medicines. Consulting a doctor ensures that other medicines you are taking won’t interfere with the treatment. Always inform your healthcare provider about other medicines to avoid potential complications.
What does tranexamic acid do for skin?
Tranexamic acid reduces hyperpigmentation and dark spots by inhibiting melanin production, which can also help address skin changes that occur during the monthly period. Many women notice fluctuations in pigmentation linked to hormonal shifts during their monthly period, and tranexamic acid can be a useful solution. By targeting melanin production, it provides consistent results, regardless of the skin changes caused by the monthly period.
What not to mix tranexamic acid with?
Avoid mixing it with products containing strong exfoliants, retinoids, or other potent actives without guidance to prevent irritation, especially if you have hereditary angioedema. People with hereditary angioedema should exercise caution when introducing new skincare products to avoid potential triggers. Always consult a dermatologist if you have hereditary angioedema or other underlying conditions before trying potent skincare ingredients.
What are the disadvantages of tranexamic acid on skin?
Potential drawbacks include skin irritation, redness, or sensitivity, especially in high concentrations, which is a consideration even with a common brand. Using a common brand with a trusted formulation may reduce the likelihood of adverse reactions. Always patch-test a common brand product before full application to ensure compatibility with your skin.
Which is better, niacinamide or tranexamic acid?
Niacinamide is better for overall skin health and barrier support, while systematic review findings suggest that tranexamic acid is more targeted for treating hyperpigmentation. According to a systematic review, niacinamide offers broad benefits for improving skin texture and hydration. Meanwhile, a systematic review highlights the efficacy of tranexamic acid in reducing melasma and dark spots.
What is the mechanism of action of tranexamic acid?
Tranexamic acid inhibits plasminogen activation, reducing fibrinolysis and stabilizing blood clots—ensure to take it as soon as prescribed for maximum effectiveness. If you miss a dose, take it as soon as you remember, unless it’s close to your next dose. It is important to take it as soon as possible when bleeding occurs to achieve optimal results.
How does tranexamic acid work to stop bleeding?
It prevents the breakdown of blood clots by blocking plasmin formation, reducing blood loss, as confirmed in double blind studies. The double blind methodology ensures unbiased evaluation of its efficacy in controlling bleeding. Many double blind trials have demonstrated its safety and effectiveness in managing excessive blood loss.
How does tranexamic acid affect blood clotting?
It stabilizes blood clots by inhibiting the enzyme plasmin, which dissolves clots. If you miss a dose, it is generally advised to take it as soon as you remember, but if it’s close to the next dose skip the missed one. Always follow your doctor’s instructions, especially if they suggest that for safety, the next dose skip may be necessary. This ensures proper medication management and reduces the risk of complications tied to skipping or doubling doses.
What are the contraindications for tranexamic acid?
Contraindications include active thromboembolic disease, as tranexamic acid is an antifibrinolytic agent that stabilizes blood clots. A history of stroke may also contraindicate the use of this antifibrinolytic agent due to its effect on clot formation. Additionally, severe renal impairment is a concern when prescribing an antifibrinolytic agent like tranexamic acid, as it is processed through the kidneys.
Does tranexamic acid work for melasma?
Yes, it is effective in reducing melasma by inhibiting melanin production and reducing pigmentation, which is especially helpful during pregnancy. Many women experience melasma during pregnancy, known as the “mask of pregnancy,” and tranexamic acid can offer a solution. However, it is important to consult with a healthcare provider before using tranexamic acid during pregnancy to ensure it is safe for both mother and baby.
Which is better, hydroquinone or tranexamic acid?
Hydroquinone is more potent for severe hyperpigmentation but carries a higher risk of side effects, which could make the condition worse if not monitored closely. On the other hand, tranexamic acid is gentler and less likely to cause irritation, making it suitable for prolonged use without making the skin condition worse. However, in some cases, if overused, tranexamic acid could potentially make the pigmentation worse, so it’s important to follow usage recommendations.
How long does it take tranexamic acid to fade dark spots?
Visible improvements in dark spots on the skin can occur within 4–8 weeks of consistent use, and the mouth area may also benefit from treatments like tranexamic acid for oral pigmentation. If you’re looking to target dark spots on the face, including around the mouth, regular use of tranexamic acid can help fade them over time. For those with pigmentation issues around the mouth, incorporating this ingredient into your skincare routine can provide noticeable results.
Can tranexamic acid be applied topically?
Yes, it is available in topical formulations for skin brightening and treating hyperpigmentation. However, before starting any new skincare treatment, it is a good idea to ask your doctor if tranexamic acid is right for your skin type. If you have sensitive skin or any underlying conditions, ask your doctor for personalized recommendations on how to incorporate it into your routine safely.
What does tranexamic acid do to the skin?
It reduces pigmentation and improves skin tone by blocking melanin pathways, which can be supported by consuming food rich in antioxidants. Certain food sources, like citrus fruits and leafy greens, can enhance the skin’s response to tranexamic acid. Combining tranexamic acid with a healthy diet full of nutrient-dense food helps promote overall skin health and radiance.
Is 10% tranexamic acid safe for skin?
Yes, but it may cause irritation in sensitive skin, affecting the skin’s ability to heal properly, which could stress the brain. Lower concentrations are often preferred, as they help minimize any adverse reactions, allowing the brain to focus on normal recovery without external stress. It’s important to monitor your skin’s response to ensure it doesn’t impact your overall well-being or cause unnecessary strain on the brain.
Can tranexamic acid be used as a mouthwash?
Yes, it can be used to reduce bleeding after dental procedures. Yes, it can be used to reduce bleeding after dental procedures, helping to maintain moisture in the affected area. Tranexamic acid aids in controlling bleeding while preserving moisture, which is important for promoting healing. Ensuring adequate moisture in the mouth can also prevent dryness and discomfort during recovery.
How do you make tranexamic acid gargle?
A doctor or pharmacist may prepare a diluted solution for use as a gargle to control oral bleeding, similar to how aspirin is sometimes used to reduce inflammation and pain. In some cases, aspirin can also be recommended for its blood-thinning properties, but it is important to consult with a healthcare provider before using aspirin or any other medication for oral bleeding. While aspirin may help in managing certain conditions, it is crucial to follow professional advice regarding its use alongside treatments like tranexamic acid for oral bleeding.
What is tranexamic acid used for in dentistry?
It is used to control bleeding during or after dental surgeries, especially in patients with bleeding disorders, including children. Tranexamic acid can also be beneficial for children who are undergoing dental procedures where there is a risk of excessive bleeding. However, it’s important to consult a healthcare provider before administering tranexamic acid to children to ensure its safety and appropriate dosage.
Is there a mouthwash that stops bleeding?
Tranexamic acid mouthwash is specifically used to reduce oral bleeding.
What can you not mix with tranexamic acid?
Avoid combining it with medications or substances that increase clotting risk without medical advice.
How long does it take for topical TXA to work?
It may take 4–12 weeks of regular use to see significant improvements in hyperpigmentation.
Reference
Bala HR, Lee S, Wong C, Pandya AG, Rodrigues M. Oral Tranexamic Acid for the Treatment of Melasma: A Review. Dermatol Surg. 2018 Jun;44(6):814-825. doi: 10.1097/DSS.0000000000001518. PMID: 29677015.
Oral Tranexamic Acid for the Treatment of Melasma
Melasma is a common hyperpigmentation disorder, particularly in individuals with skin of color, and tranexamic acid (TXA) has emerged as an effective treatment option. [1] Oral TXA, even at low doses (500 mg daily), has shown efficacy in improving melasma within 8–12 weeks, with a favorable safety profile and minimal side effects. It is recommended for refractory cases unresponsive to topical treatments, provided patients are screened for contraindications and thromboembolic risk factors.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/29677015/.
Ebrahimi B, Naeini FF. Topical tranexamic acid as a promising treatment for melasma. J Res Med Sci. 2014 Aug;19(8):753-7. PMID: 25422661; PMCID: PMC4235096.
Topical tranexamic acid as a promising treatment for melasma
Gaćina K, Krstanović Ćosić A. THE USE OF TRANEXAMIC ACID IN DERMATOLOGY. Acta Clin Croat. 2023 Aug;62(2):368-372. doi: 10.20471/acc.2023.62.02.16. PMID: 38549597; PMCID: PMC10969640.
THE USE OF TRANEXAMIC ACID IN DERMATOLOGY
Tranexamic acid, a synthetic derivative of lysine, is primarily used to reduce bleeding in surgical, trauma, and dental settings. Its anti-inflammatory and melanin-suppressing properties make it effective in treating dermatological conditions like melasma, acne, post-inflammatory hyperpigmentation, and rosacea through oral, topical, or injectable routes. This review highlights its versatility and efficacy in managing various skin disorders.
You can read the abstract of this article at
https://pmc.ncbi.nlm.nih.gov/articles/PMC10969640/Tan AWM, Sen P, Chua SH, Goh BK. Oral tranexamic acid lightens refractory melasma. Australas J Dermatol. 2017 Aug;58(3):e105-e108. doi: 10.1111/ajd.12474. Epub 2016 May 13. PMID: 27173008.
Oral tranexamic acid lightens refractory melasma. Australas J Dermatol
This study evaluated the effectiveness of low-dose oral tranexamic acid (250 mg twice daily) as an adjunct therapy for refractory melasma in 25 patients. Results showed a significant 69% improvement in melasma severity, with mean MASI scores decreasing from 8.8 to 2.7 after 3.7 months of treatment (P < 0.01). The findings suggest oral tranexamic acid is a safe and effective option for managing melasma unresponsive to topical treatments.You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/27173008/.Anwar AI, Wahab S, Widita W, Nurdin AR, Budhiani S, Seweng A. Randomized control trial outcomes of tranexamic acid combination serum as a depigmenting agent for the use in healthy individuals. Dermatol Ther. 2019 Nov;32(6):e13146. doi: 10.1111/dth.13146. Epub 2019 Nov 13. PMID: 31664751.
Cho YH, Park JE, Lim DS, Lee JS. Tranexamic acid inhibits melanogenesis by activating the autophagy system in cultured melanoma cells. J Dermatol Sci. 2017 Oct;88(1):96-102. doi: 10.1016/j.jdermsci.2017.05.019. Epub 2017 Jun 7. PMID: 28669590.
Tranexamic acid inhibits melanogenesis by activating the autophagy system in cultured melanoma cells
Tranexamic acid (TXA) has been shown to reduce melanin synthesis in melanoma B16-F1 cells by activating the autophagy system and the ERK signaling pathway. The study demonstrated that TXA enhances autophagy-related protein production while downregulating melanogenesis-associated proteins, including tyrosinase and MITF, leading to decreased melanin production. These findings suggest TXA’s potential as a mechanism-based skin-whitening agent.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/28669590/.Furmanczyk M, Brown A, Bustos J, de Henestrosa ARF, Trullas C, Granger C, Jourdan E. Efficacy and tolerability of a depigmenting gel serum comprising tranexamic acid, niacinamide, 4-butylresorcinol, phytic acid, and a mixture of hydroxy acids that targets the biological processes regulating skin melanogenesis. J Cosmet Dermatol. 2024 Jun;23(6):2058-2065. doi: 10.1111/jocd.16148. Epub 2024 Mar 28. PMID: 38549196.
Efficacy and tolerability of a depigmenting gel serum comprising tranexamic acid, niacinamide, 4-butylresorcinol, phytic acid, and a mixture of hydroxy acids that targets the biological processes regulating skin melanogenesis
This study evaluated a gel serum containing tranexamic acid, niacinamide, 4-butylresorcinol, phytic acid, and hydroxy acids for its ability to reduce hyperpigmentation by targeting melanogenesis. Results showed significant reductions in melanin production and brown spots within 14 days, with improvements sustained throughout treatment and maintained one month after cessation. The product demonstrated excellent skin tolerability, making it an effective and safe option for managing hyperpigmentation.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/38549196/.Liu LX, Liao ZK, Dong BQ, Jiang S, Lei TC. Tranexamic Acid Ameliorates Skin Hyperpigmentation by Downregulating Endothelin-1 Expression in Dermal Microvascular Endothelial Cells. Ann Dermatol. 2024 Jun;36(3):151-162. doi: 10.5021/ad.23.108. PMID: 38816976; PMCID: PMC11148312.
Tranexamic Acid Ameliorates Skin Hyperpigmentation by Downregulating Endothelin-1 Expression in Dermal Microvascular Endothelial Cells
This study compares the skin-lightening effects of oral and topical tranexamic acid (TXA) in a UVB-induced hyperpigmentation mouse model and human skin samples. The results indicate that oral TXA is more effective than topical TXA in reducing hyperpigmentation by suppressing endothelin-1 (ET-1) production in vascular endothelial cells, which decreases melanogenesis and melanocyte proliferation. These findings highlight the superior efficacy of oral TXA in skin lightening through its impact on dermal microvascular pathways.
You can read the abstract of this article at
https://pmc.ncbi.nlm.nih.gov/articles/PMC11148312/.Kim KM, Lim HW. The uses of tranexamic acid in dermatology: a review. Int J Dermatol. 2023 May;62(5):589-598. doi: 10.1111/ijd.16160. Epub 2022 Mar 24. PMID: 35323992.
The uses of tranexamic acid in dermatology: a review
Tranexamic acid, a plasmin inhibitor, is used off-label in dermatology for treating conditions like melasma, rosacea, and post-inflammatory hyperpigmentation due to its anti-inflammatory and anti-melanin properties. While it shows promise for broader applications, caution is advised during the COVID-19 pandemic due to its procoagulant effects. Further studies are needed to explore its full potential in dermatology.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/35323992/.Visit at https://www.mdpi.com/2079-9284/11/5/168.
Visit at https://onlinelibrary.wiley.com/doi/10.1111/jocd.15786.
Ebrahimi B, Naeini FF. Topical tranexamic acid as a promising treatment for melasma. J Res Med Sci. 2014 Aug;19(8):753-7. PMID: 25422661; PMCID: PMC4235096.
Topical tranexamic acid as a promising treatment for melasma
The study evaluated the efficacy and safety of topical tranexamic acid (TA) compared to a combination of hydroquinone and dexamethasone in treating melasma in Iranian women. Both treatments significantly reduced the Melasma Area and Severity Index (MASI) scores with similar satisfaction levels, but TA had fewer side effects. The findings suggest TA is a safe and effective alternative for melasma treatment.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/25422661/.Maeda K. Timeline of the Development of Skin-Lightening Active Ingredients in Japan. Molecules. 2022 Jul 26;27(15):4774. doi: 10.3390/molecules27154774. PMID: 35897958; PMCID: PMC9369694.
Timeline of the Development of Skin-Lightening Active Ingredients in Japan
Japanese pharmaceutical cosmetics, or quasi-drugs, use active ingredients like arbutin and rucinol to prevent pigmentation by suppressing melanin production, while others like disodium adenosine monophosphate reduce melanin accumulation. Oral products containing vitamin C and tranexamic acid are more effective for treating freckles and melasma compared to quasi-drugs. This review categorizes skin-lightening ingredients by effectiveness and side effects, highlighting Japan’s advancements in this field.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/35897958/.Visit at https://onlinelibrary.wiley.com/doi/10.1111/jocd.16332.
Wu S, Shi H, Wu H, Yan S, Guo J, Sun Y, Pan L. Treatment of melasma with oral administration of tranexamic acid. Aesthetic Plast Surg. 2012 Aug;36(4):964-70. doi: 10.1007/s00266-012-9899-9. Epub 2012 May 3. PMID: 22552446.
Treatment of melasma with oral administration of tranexamic acid
Oral tranexamic acid (TA) was studied as a treatment for melasma in 74 Chinese patients, with a dosage of 250 mg twice daily over six months. Results showed improvement in pigmentation and melasma size, with 64.8% rated as excellent or good, though mild side effects like gastrointestinal discomfort and hypomenorrhea were noted. The study concluded that TA is a safe and effective therapy for melasma, with minimal recurrence observed.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/22552446/.Desai S, Ayres E, Bak H, Manco M, Lynch S, Raab S, Du A, Green D, Skobowiat C, Wangari-Talbot J, Zheng Q. Effect of a Tranexamic Acid, Kojic Acid, and Niacinamide Containing Serum on Facial Dyschromia: A Clinical Evaluation. J Drugs Dermatol. 2019 May 1;18(5):454-459. PMID: 31141852.
Effect of a Tranexamic Acid, Kojic Acid, and Niacinamide Containing Serum on Facial Dyschromia: A Clinical Evaluati
This study evaluated the effectiveness of a topical serum containing 3% tranexamic acid, 1% kojic acid, and 5% niacinamide in treating melasma, post-inflammatory hyperpigmentation (PIH), and hyperpigmentation over 12 weeks in Brazilian women. Results showed significant improvements in pigmentation, skin tone, and texture starting at week 2, with continued progress through week 12, as confirmed by clinical assessments and melanin measurements. The serum was found to be an effective and well-tolerated treatment option for hyperpigmentary conditions, potentially acting by inhibiting inflammatory mediators involved in melanogenesis.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/31141852/.Juhasz MLW, Levin MK. The role of systemic treatments for skin lightening. J Cosmet Dermatol. 2018 Dec;17(6):1144-1157. doi: 10.1111/jocd.12747. Epub 2018 Aug 21. PMID: 30133125.
The role of systemic treatments for skin lightening
Systemic therapies for skin lightening, such as oral carotenoids, glutathione, melatonin, and tranexamic acid, show promise in treating hyperpigmentation conditions like melasma and post-inflammatory hyperpigmentation. While these treatments are generally safe, intravenous glutathione is discouraged due to potential adverse effects. Dermatologists must understand the efficacy and safety profiles of these therapies to counsel patients effectively on treatment expectations and proper use.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/30133125/.Shimshak SJE, Tolaymat LM, Haga CB, Dawson NL, Gillis MS, Yin M, Kirsch B, Cooper M, Sluzevich JC. A Review of Oral Therapies for the Treatment of Skin Hyperpigmentation. J Cutan Med Surg. 2022 Mar-Apr;26(2):169-175. doi: 10.1177/12034754211045391. Epub 2021 Sep 19. PMID: 34541912.
A Review of Oral Therapies for the Treatment of Skin Hyperpigmentation
This review explores the effectiveness of oral therapies, such as tranexamic acid, glutathione, isotretinoin, and proanthocyanidin, in treating various types of skin hyperpigmentation. While these treatments show promise, their efficacy depends on addressing underlying causes like hormonal imbalances or metabolic conditions, and results for idiopathic cases are less predictable. Limitations include small sample sizes, lack of blinding, and a need for further research to confirm safety and effectiveness.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/34541912/.Kalasho BD, Minokadeh A, Zhang-Nunes S, Zoumalan RA, Shemirani NL, Waldman AR, Pletzer V, Zoumalan CI. Evaluating the Safety and Efficacy of a Topical Formulation Containing Epidermal Growth Factor, Tranexamic Acid, Vitamin C, Arbutin, Niacinamide and Other Ingredients as Hydroquinone 4% Alternatives to Improve Hyperpigmentation: A Prospective, Randomized, Controlled Split Face Study. J Cosmet Sci. 2020 Sep/Oct;71(5):263-290. PMID: 33022197.
Evaluating the Safety and Efficacy of a Topical Formulation Containing Epidermal Growth Factor, Tranexamic Acid, Vitamin C, Arbutin, Niacinamide and Other Ingredients as Hydroquinone 4% Alternatives to Improve Hyperpigmentation: A Prospective, Randomized, Controlled Split Face Study
This study evaluated the safety and efficacy of SKNB19, a non-hydroquinone (HQ) topical formulation, in treating hyperpigmentation compared to hydroquinone 4% (HQ4%). Results showed SKNB19 significantly improved hyperpigmentation appearance by 28.5% (self-assessment) and 27% (independent assessment) over HQ4% while causing fewer adverse effects and being better tolerated. These findings suggest SKNB19 is a safe and effective alternative to HQ for managing hyperpigmentation.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/33022197/.Zhao H, Li M, Zhang X, Li L, Yan Y, Wang B. Comparing the efficacy of Myjet-assisted tranexamic acid and vitamin C in treating melasma: A split-face controlled trial. J Cosmet Dermatol. 2020 Jan;19(1):47-54. doi: 10.1111/jocd.13112. Epub 2019 Sep 3. PMID: 31479196.
Comparing the efficacy of Myjet-assisted tranexamic acid and vitamin C in treating melasma: A split-face controlled trial
This study compared the efficacy and safety of transdermal injections of tranexamic acid (TA) and vitamin C (VC) in treating melasma. Both treatments showed a significant reduction in MASI scores, with no statistically significant difference between the two. The treatments were well tolerated, with no serious side effects, suggesting that weekly TA or VC injections can be effective for melasma, although further research is needed.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/31479196/.Visit at https://www.mdpi.com/2079-9284/9/5/108.
Kaikati J, El Bcherawi N, Khater JA, Dib SM, Kechichian E, Helou J. Combination Topical Tranexamic Acid and Vitamin C for the Treatment of Refractory Melasma. J Clin Aesthet Dermatol. 2023 Jul;16(7):63-65. PMID: 37560507; PMCID: PMC10409511.
Combination Topical Tranexamic Acid and Vitamin C for the Treatment of Refractory Melasma
This pilot study evaluated the effectiveness of a topical combination of 2% tranexamic acid (TA) and 2% vitamin C in treating resistant melasma in 10 women from the Mediterranean region. The results showed significant improvements in melasma severity, with the Melasma Area and Severity Index (MASI) score decreasing from 12.76 at baseline to 3.39 by Week 8. The treatment also led to a reduction in the Melasma Quality of Life Scale (MelasQoL) score and no major side effects were reported, suggesting this combination could be a safe and effective alternative to harsher treatments for melasma.
You can read the abstract of this article at
https://pmc.ncbi.nlm.nih.gov/articles/PMC10409511/.da Silva Souza ID, Lampe L, Winn D. New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin. J Cosmet Dermatol. 2021 Feb;20(2):561-565. doi: 10.1111/jocd.13545. Epub 2020 Jun 25. PMID: 32588531.
New topical tranexamic acid derivative for the improvement of hyperpigmentation and inflammation in the sun-damaged skin
A facial serum containing 2.0% cetyl tranexamate mesylate was tested for its safety and skin-lightening effects in a study with 54 participants. The results showed significant improvements in melanin and erythema indexes, with subjects reporting better skin tone, reduced dark spots, and less facial redness after 2 weeks of use. The serum was well-tolerated, with no adverse reactions observed, making it an effective option for improving skin appearance and treating pigmentation issues.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/32588531/.Charoenwattanayothin A, Saiwichai T, Chaichalotornkul S. Adjunctive treatment for acne vulgaris by tranexamic acid. J Cosmet Dermatol. 2022 Oct;21(10):4515-4522. doi: 10.1111/jocd.14972. Epub 2022 May 10. PMID: 35388589.
Adjunctive treatment for acne vulgaris by tranexamic acid
A study evaluated the efficacy of 10% tranexamic acid (TXA) serum in treating mild-to-moderate acne, finding significant reductions in inflammatory acne, particularly papules and pustules, after 8 weeks of use. TXA also decreased skin redness and post-inflammatory erythema (PIE) and hyperpigmentation (PIH), with minimal and treatable side effects. The results suggest that topical 10% TXA is an effective treatment for inflammatory acne with minor adverse effects.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/35388589/.Jakhar D, Kaur I. Topical 5% tranexamic acid for acne-related postinflammatory erythema. J Am Acad Dermatol. 2020 Jun;82(6):e187-e188. doi: 10.1016/j.jaad.2019.09.074. Epub 2019 Oct 4. PMID: 31589950.
Topical 5% tranexamic acid for acne-related postinflammatory erythema
Topical 5% tranexamic acid (TXA) is an effective, well-tolerated treatment for reducing postinflammatory erythema (PIE) when applied nightly, with visible improvements within 6–8 weeks. Its ease of use, lack of significant side effects, and ability to address skin redness make it a promising option for managing PIE and other erythema-related conditions.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/31589950/.Sobhan M, Talebi-Ghane E, Poostiyan E. A comparative study of 20% azelaic acid cream versus 5% tranexamic acid solution for the treatment of postinflammatory hyperpigmentation in patients with acne vulgaris: A single-blinded randomized clinical trial. J Res Med Sci. 2023 Apr 1;28:18. doi: 10.4103/jrms.jrms_443_22. PMID: 37213446; PMCID: PMC10199364.
A comparative study of 20% azelaic acid cream versus 5% tranexamic acid solution for the treatment of postinflammatory hyperpigmentation in patients with acne vulgaris: A single-blinded randomized clinical trial
This study compared the efficacy of 20% azelaic acid (AZA) cream and 5% tranexamic acid (TA) solution for treating acne-related postinflammatory hyperpigmentation (PIH). Both treatments showed similar improvements in the postacne hyperpigmentation index (PAHI) scores over 12 weeks, with no significant difference between the groups. However, TA had a better safety profile, with fewer side effects reported, particularly in the first month of treatment.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/37213446/.Lindgren AL, Austin AH, Welsh KM. The Use of Tranexamic Acid to Prevent and Treat Post-Inflammatory Hyperpigmentation. J Drugs Dermatol. 2021 Mar 1;20(3):344-345. doi: 10.36849/JDD.5622. PMID: 33683077.
The Use of Tranexamic Acid to Prevent and Treat Post-Inflammatory Hyperpigmentation
Post-inflammatory hyperpigmentation (PIH) is a common complication after dermatologic procedures like laser treatments and chemical peels, and it can also result from conditions such as acne and burns. High-risk patients, including those with Fitzpatrick skin types 3–5 or a history of PIH, are more likely to develop this condition. Tranexamic acid (TXA), an antifibrinolytic medication, has been used off-label to successfully treat and prevent PIH in high-risk patients, including those undergoing procedures like microneedling, cryotherapy, and chemical peels, with TXA being administered prophylactically in many cases.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/33683077/.Tawfic SO, Abdel Hay R, Salim H, Elmasry MF. Tranexamic acid versus fractional carbon dioxide laser in post-acne hyperpigmentation. Dermatol Ther. 2021 Nov;34(6):e15103. doi: 10.1111/dth.15103. Epub 2021 Sep 6. PMID: 34414642.
Tranexamic acid versus fractional carbon dioxide laser in post-acne hyperpigmentation
This study compared the efficacy of low-power fractional CO2 laser and tranexamic acid (TXA) microinjection for treating post-acne hyperpigmentation in patients resistant to regular treatments. Both treatments showed significant improvement in pigmentation, but fractional CO2 laser demonstrated better results, particularly in dermoscopic scores. The study concluded that both methods are effective and safe, with fractional CO2 laser potentially offering superior results for post-acne hyperpigmentation.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/34414642/.Bazargan AS, Ziaeifar E, Abouie A, Mirahmadi S, Taheri A, Gheisari M. Evaluating the effect of tranexamic acid as mesotherapy on persistent post-acne erythema: A before and after study. J Cosmet Dermatol. 2023 Oct;22(10):2714-2720. doi: 10.1111/jocd.15776. Epub 2023 Apr 21. PMID: 37082869.
Evaluating the effect of tranexamic acid as mesotherapy on persistent post-acne erythema: A before and after study
This study evaluated the efficacy of tranexamic acid (TA) mesotherapy for treating post-acne erythema (PAE) in 17 patients. Results showed significant improvement in lesion count, area, and area percent on the treated side, with no notable changes on the control side. While TA injections appear effective for PAE, further research with larger sample sizes is needed to confirm these findings.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/37082869/.Gaćina K, Krstanović Ćosić A. THE USE OF TRANEXAMIC ACID IN DERMATOLOGY. Acta Clin Croat. 2023 Aug;62(2):368-372. doi: 10.20471/acc.2023.62.02.16. PMID: 38549597; PMCID: PMC10969640.
THE USE OF TRANEXAMIC ACID IN DERMATOLOGY
Tranexamic acid, a synthetic derivative of lysine, is primarily used to reduce bleeding in medical and dental procedures but has found applications in dermatology for conditions like melasma, acne, and rosacea due to its anti-inflammatory and melanogenesis-suppressing properties. It can be administered orally, topically, or via intradermal injection, often in combination with other treatments. This review highlights evidence supporting its effectiveness in treating various skin disorders.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/38549597/Chen T, Xue J, Wang Q. Tranexamic Acid for the Treatment of Hyperpigmentation and Telangiectatic Disorders Other Than Melasma: An Update. Clin Cosmet Investig Dermatol. 2024 Sep 25;17:2151-2163. doi: 10.2147/CCID.S479411. PMID: 39350932; PMCID: PMC11439988.
Tranexamic Acid for the Treatment of Hyperpigmentation and Telangiectatic Disorders Other Than Melasma: An Update
Tranexamic acid (TXA), a synthetic antifibrinolytic agent, is widely used for controlling bleeding in trauma, surgeries, and hemophilia. Beyond its hemostatic applications, TXA has shown potential in treating hyperpigmentation and telangiectatic disorders through anti-inflammatory and skin barrier-repair effects, with oral, topical, and injectable modes of administration. While most research focuses on melasma, emerging evidence supports its use in conditions like post-inflammatory hyperpigmentation, rosacea, and post-acne erythema, offering safer and cost-effective treatment options.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/39350932/.Zhang J, Gu D, Yan Y, Pan R, Zhong H, Zhang C, Xu Y. Potential Role of Tranexamic Acid in Rosacea Treatment: conquering Flushing Beyond Melasma. Clin Cosmet Investig Dermatol. 2024 Jun 14;17:1405-1412. doi: 10.2147/CCID.S473598. Erratum in: Clin Cosmet Investig Dermatol. 2024 Jun 26;17:1551-1552. doi: 10.2147/CCID.S484236. PMID: 38895607; PMCID: PMC11185165.
Potential Role of Tranexamic Acid in Rosacea Treatment: conquering Flushing Beyond Melasma
Rosacea is a chronic inflammatory skin condition affecting the midface, characterized by erythema, flushing, and other symptoms. While the precise pathophysiology remains unclear, tranexamic acid (TA), known for treating melasma and other skin conditions, has shown promise in alleviating rosacea symptoms through mechanisms like barrier restoration and angiogenesis inhibition. This review explores the therapeutic potential of TA for rosacea via various delivery methods, including oral, topical, and advanced techniques like microneedling and laser-assisted delivery.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/38895607/.Xu Z, Yu B, Xu B, Ye S, Qing Y, Zhao B, Hong S, Wu N, Wu J. Oral tranexamic acid treats papulopustular rosacea by improving the skin barrier. J Cosmet Dermatol. 2024 Sep;23(9):2918-2926. doi: 10.1111/jocd.16339. Epub 2024 May 7. PMID: 38712728.
Oral tranexamic acid treats papulopustular rosacea by improving the skin barrier
Tranexamic acid (TXA) has shown promising results in treating papulopustular rosacea (PPR) by enhancing skin barrier function, reducing dryness, and improving overall skin hydration. A study involving 70 patients demonstrated that adding oral TXA to traditional therapy significantly improved clinical outcomes, patient satisfaction, and quality of life compared to traditional therapy alone, with better results observed in dry-type rosacea. TXA was well-tolerated, with no significant side effects reported.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/38712728/.Li Y, Xie H, Deng Z, Wang B, Tang Y, Zhao Z, Yuan X, Zuo Z, Xu S, Zhang Y, Li J. Tranexamic acid ameliorates rosacea symptoms through regulating immune response and angiogenesis. Int Immunopharmacol. 2019 Feb;67:326-334. doi: 10.1016/j.intimp.2018.12.031. Epub 2018 Dec 19. PMID: 30578968.
Tranexamic acid ameliorates rosacea symptoms through regulating immune response and angiogenesis
Tranexamic acid (TXA) has emerged as an effective treatment for rosacea by regulating immune responses and angiogenesis. In LL37-induced mouse and HaCaT cell models, TXA reduced skin erythema, pro-inflammatory cytokines (IL-6, TNFα), and angiogenesis markers like VEGF, while modulating both innate and adaptive immune responses. These findings highlight TXA’s therapeutic potential in mitigating inflammation and vascular hyperreactivity in rosacea.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/30578968/.Bageorgou F, Vasalou V, Tzanetakou V, Kontochristopoulos G. The new therapeutic choice of tranexamic acid solution in treatment of erythematotelangiectatic rosacea. J Cosmet Dermatol. 2019 Apr;18(2):563-567. doi: 10.1111/jocd.12724. Epub 2018 Aug 11. PMID: 30099833.
The new therapeutic choice of tranexamic acid solution in treatment of erythematotelangiectatic rosacea
The study evaluated the efficacy of topical tranexamic acid for treating erythematotelangiectatic rosacea in 20 women aged 27–65 years. Patients treated with tranexamic acid alone or combined with microneedling showed significant improvement, with better outcomes in the combined treatment group. The therapy was well-tolerated, effective, and offers a promising, safe, and cost-effective option for managing rosacea symptoms.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/30099833/.Mohamed RR, Mahmoud Mohamed LG, Mansour M, Rageh MA. Topical 10% Tranexamic Acid with and without Microneedling in the Treatment of Erythematotelangiectatic Rosacea: A Split-face Comparative Study. J Clin Aesthet Dermatol. 2024 Feb;17(2):47-51. PMID: 38444423; PMCID: PMC10911261.
Topical 10% Tranexamic Acid with and without Microneedling in the Treatment of Erythematotelangiectatic Rosacea: A Split-face Comparative Study
This study evaluated the efficacy of 10% topical tranexamic acid (TXA) with and without microneedling for treating erythematotelangiectatic rosacea (ETR). Both treatments showed improvement, but combining TXA with microneedling resulted in significantly better outcomes for reducing erythema and telangiectasia. The study concludes that TXA is effective and safe, with microneedling enhancing its delivery and efficacy.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/38444423/.Daadaa N, Litaiem N, Karray M, Bacha T, Jones M, Belajouza Noueiri C, Goucha S, Zeglaoui F. Intradermal tranexamic acid microinjections: a novel treatment option for erythematotelangiectatic rosacea. J Cosmet Dermatol. 2021 Oct;20(10):3324-3329. doi: 10.1111/jocd.14209. Epub 2021 May 25. PMID: 33973361.
Intradermal tranexamic acid microinjections: a novel treatment option for erythematotelangiectatic rosacea
Intradermal microinjections of tranexamic acid (TXA) were evaluated as a treatment for erythematotelangiectatic rosacea (ETR) in a retrospective study of six patients. Results showed a significant reduction in rosacea severity scores, with transient local side effects but no systemic effects. TXA microinjections appear to be a safe and effective option for ETR, though the optimal treatment schedule requires further study.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/33973361/.Peruzzo J, Barea P, Crusius DVS, Brum LF, Cionek OAGD, Fiegenbaum AB, Boza JC, Bonamigo RR. Clinical evaluation and quality of life following the use of tranexamic acid in rosacea. Arch Dermatol Res. 2024 Oct 26;316(10):720. doi: 10.1007/s00403-024-03476-1. PMID: 39460756.
Clinical evaluation and quality of life following the use of tranexamic acid in rosacea
A study published in Archives of Dermatological Research evaluated the clinical efficacy and impact on quality of life of tranexamic acid (TXA) in patients with rosacea. The findings suggest that TXA treatment may offer benefits for rosacea management.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/39460756/.Jakhar D, Kaur I, Misri R. Topical 10% tranexamic acid for erythematotelangiectatic steroid-induced rosacea. J Am Acad Dermatol. 2022 Jan;86(1):e1-e2. doi: 10.1016/j.jaad.2019.12.067. Epub 2020 Jan 11. PMID: 31931084.
- Topical 10% tranexamic acid for erythematotelangiectatic steroid-induced rosaceaTopical application of 10% tranexamic acid (TXA) has been found to significantly reduce erythema, telangiectasia, and burning sensations associated with steroid-induced rosacea within 4 to 6 weeks of treatment. This approach is noted for its ease of preparation and favorable tolerability profile.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/31931084/.
- Topical 10% tranexamic acid for erythematotelangiectatic steroid-induced rosaceaTopical application of 10% tranexamic acid (TXA) has been found to significantly reduce erythema, telangiectasia, and burning sensations associated with steroid-induced rosacea within 4 to 6 weeks of treatment. This approach is noted for its ease of preparation and favorable tolerability profile.
Tang J, Li Y, Hu X, Hua W, Xu H, Li L, Xu F. Enhancing Tranexamic Acid Penetration through AQP-3 Protein Triggering via ZIF-8 Encapsulation for Melasma and Rosacea Therapy. Adv Healthc Mater. 2024 Jul;13(17):e2304189. doi: 10.1002/adhm.202304189. Epub 2024 Apr 24. PMID: 38539056.
Enhancing Tranexamic Acid Penetration through AQP-3 Protein Triggering via ZIF-8 Encapsulation for Melasma and Rosacea Therapy
A novel topical application of tranexamic acid (TA) using TA-loaded ZIF-8 (TA@ZIF-8) enhances its penetration through the skin barrier and addresses limitations of systemic use and traditional transdermal delivery methods. TA@ZIF-8 improves drug encapsulation, intracellular uptake, and activates the aquaporin-3 protein, resulting in effective treatment of melasma and rosacea with minimal cytotoxicity. Clinical trials confirm its safety and efficacy, presenting a promising alternative to systemic administration for anti-inflammatory and anti-pigmentation therapies.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/38539056/.Agamia N, El-Nagdy S, El-Ariny A. A split face comparative study using a novel triple combination therapy for the treatment of persistent post acne erythema. Dermatol Ther. 2022 Apr;35(4):e15327. doi: 10.1111/dth.15327. Epub 2022 Jan 31. PMID: 35060229.
A split face comparative study using a novel triple combination therapy for the treatment of persistent post acne erythema
The study evaluated the efficacy and safety of a topical triple combination (tranexamic acid 5%, oxymetazoline 1.5%, and brimonidine tartrate 0.33%) for treating persistent post-acne erythema (PAE) in a split-face study involving 40 patients over three months. Results showed that the combination treatment significantly reduced PAE on the treated side compared to the placebo, confirming it as a safe and cost-effective option. The findings highlight its potential as an innovative therapy for addressing PAE.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/35060229/.Frank MM, Zuraw B, Banerji A, Bernstein JA, Craig T, Busse P, Christiansen S, Davis-Lorton M, Li HH, Lumry WR, Riedl M; US Hereditary Angioedema Association Medical Advisory Board. Management of Children With Hereditary Angioedema Due to C1 Inhibitor Deficiency. Pediatrics. 2016 Nov;138(5):e20160575. doi: 10.1542/peds.2016-0575. PMID: 27940765.
Management of Children With Hereditary Angioedema Due to C1 Inhibitor Deficiency
Hereditary angioedema (HAE) is a life-threatening inherited condition characterized by swelling attacks, often starting in childhood, that are unresponsive to standard allergy treatments. While effective treatments exist for adults, options for children under 12 are limited, with only one approved medication. The Medical Advisory Board, in collaboration with the HAE Patient’s Association, has developed consensus recommendations to guide the recognition, diagnosis, and treatment of HAE in children.
You can read the abstract of this article at
https://pubmed.ncbi.nlm.nih.gov/27940765/.Milingos DS, Madhuvrata P, Dean J, Shetty A, Campbell DM. Hereditary angioedema and pregnancy: successful management of recurrent and frequent attacks of angioedema with C1-inhibitor concentrate, danazol and tranexamic acid – a case report. Obstet Med. 2009 Sep;2(3):123-5. doi: 10.1258/om.2009.090003. Epub 2009 Sep 1. PMID: 27582827; PMCID: PMC4989748.
Hereditary angioedema and pregnancy: successful management of recurrent and frequent attacks of angioedema with C1-inhibitor concentrate, danazol and tranexamic acid – a case report
Hereditary angioedema (HAE) is a rare, life-threatening condition caused by C1 esterase inhibitor deficiency, leading to swelling in the skin, gastrointestinal, and respiratory tracts. This case highlights a pregnant woman with worsening HAE, managed effectively with danazol, tranexamic acid, and regular intravenous C1 esterase inhibitor therapy.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/27582827/.Ohela K. Treatment of hereditary angioneurotic edema with tranexamic acid and cinnarizine. Acta Derm Venereol. 1976;56(1):61-7. PMID: 56859.
Treatment of hereditary angioneurotic edema with tranexamic acid and cinnarizine
Tranexamic acid (AMCA) effectively managed hereditary angioneurotic edema in six out of seven Finnish patients, with some achieving near symptom-free status on continuous treatment. However, one patient discontinued AMCA due to fatigue and nausea. In comparison, antihistamine treatment with cinnarizine also helped two out of three patients by reducing attack frequency and severity.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/56859/.Wintenberger C, Boccon-Gibod I, Launay D, Fain O, Kanny G, Jeandel PY, Martin L, Gompel A, Bouillet L. Tranexamic acid as maintenance treatment for non-histaminergic angioedema: analysis of efficacy and safety in 37 patients. Clin Exp Immunol. 2014 Oct;178(1):112-7. doi: 10.1111/cei.12379. PMID: 24827773; PMCID: PMC4360201.
Tranexamic acid as maintenance treatment for non-histaminergic angioedema: analysis of efficacy and safety in 37 patients
Tranexamic acid (TA) appears to be an effective and well-tolerated maintenance treatment for some patients with hereditary angioedema (HAE) or idiopathic non-histaminergic angioedema (AE), reducing attack frequency by 75% in nearly half of the patients studied over six months. The study, involving 37 cases, reported no increase in symptoms or thromboembolic events, with digestive side effects being the most common. TA offers a promising, affordable option for managing non-histaminergic AE.
You can read the abstract of this article at https://pmc.ncbi.nlm.nih.gov/articles/PMC4360201/.Longhurst H, Zinser E. Prophylactic Therapy for Hereditary Angioedema. Immunol Allergy Clin North Am. 2017 Aug;37(3):557-570. doi: 10.1016/j.iac.2017.04.003. PMID: 28687109.
Prophylactic Therapy for Hereditary Angioedema
Long-term prophylaxis for hereditary angioedema presents challenges due to side effects of current treatments. While attenuated androgens are effective, tranexamic acid and progestagens offer alternatives with fewer side effects, particularly for children and women. C1 inhibitor therapy is effective but requires intravenous administration, and new therapies show promise in addressing current limitations.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/28687109/.Marasini B, Cicardi M, Martignoni GC, Agostoni A. Treatment of hereditary angioedema. Klin Wochenschr. 1978 Aug 15;56(16):819-23. doi: 10.1007/BF01489716. PMID: 308574.
Treatment of hereditary angioedema
This study evaluated treatments for hereditary angioedema in 20 patients, focusing on the effectiveness of tranexamic acid and intravenous infusions of kallikrein inhibitor or C1 esterase inhibitor concentrate. Tranexamic acid prevented swellings in most cases without serious side effects, while C1 esterase inhibitor concentrate was highly effective for acute attacks, showing faster improvement compared to kallikrein inhibitor. Serum levels of C4 and C1 esterase inhibitor were also assessed before and after treatments.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/308574/.Calderón O, Muñoz D, Olivares M. Serie de casos de pacientes con angioedema hereditario y uso de ácido tranexámico como tratamiento profiláctico, y en crisis agudas: experiencia en Perú [Case series of hereditary angioedema patients and use of tranexamic acid treatments in prophylaxis and acute crisis, experience in Perú]. Rev Alerg Mex. 2024 Feb 1;71(1):55. Spanish. doi: 10.29262/ram.v71i1.1319. PMID: 38683073.
[Case series of hereditary angioedema patients and use of tranexamic acid treatments in prophylaxis and acute crisis, experience in Perú]
In Peru, Tranexamic Acid (TA) has been used successfully in managing hereditary angioedema (HAE) in patients for both prophylactic and acute treatment. Case studies of three women with different HAE subtypes demonstrated that TA, administered in varying oral and intravenous doses, effectively reduced symptoms and controlled acute crises, especially where specific HAE treatments were unavailable. High doses of TA were well-tolerated and showed acceptable responses, suggesting its potential as an alternative treatment in regions without registered HAE-specific therapies.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/38683073/.Cugno M, Cicardi M, Agostoni A. Activation of the contact system and fibrinolysis in autoimmune acquired angioedema: a rationale for prophylactic use of tranexamic acid. J Allergy Clin Immunol. 1994 May;93(5):870-6. doi: 10.1016/0091-6749(94)90380-8. PMID: 8182230.
Activation of the contact system and fibrinolysis in autoimmune acquired angioedema: a rationale for prophylactic use of tranexamic acid
C1-inhibitor deficiency causes mucocutaneous edema and may be hereditary or acquired, with the acquired form (AAE) responding better to antifibrinolytic agents like tranexamic acid. A study of eight patients with autoimmune AAE showed elevated levels of cleaved high molecular weight kininogen and antiplasmin-plasmin complexes in all conditions, along with inactive C1-inhibitor. Prophylactic treatment reduced symptoms but did not significantly alter these biochemical markers.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/8182230/.Wintenberger C, Boccon-Gibod I, Launay D, Fain O, Kanny G, Jeandel PY, Martin L, Gompel A, Bouillet L. Tranexamic acid as maintenance treatment for non-histaminergic angioedema: analysis of efficacy and safety in 37 patients. Clin Exp Immunol. 2014 Oct;178(1):112-7. doi: 10.1111/cei.12379. PMID: 24827773; PMCID: PMC4360201.
Tranexamic acid as maintenance treatment for non-histaminergic angioedema: analysis of efficacy and safety in 37 patients
Tranexamic acid (TA) has shown promise as a maintenance treatment for non-histaminergic angioedema (AE), including hereditary AE and idiopathic non-histaminergic AE, according to a national retrospective study. Over six months, TA reduced attacks by 75% in nearly half of the patients, with no increase in symptoms or thromboembolic events. TA is well-tolerated, cost-effective, and may benefit select AE patients, though digestive side effects were noted.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/24827773/.Wang K, Geiger H, McMahon A. Tranexamic acid for ACE inhibitor induced angioedema. Am J Emerg Med. 2021 May;43:292.e5-292.e7. doi: 10.1016/j.ajem.2020.10.029. Epub 2020 Oct 21. PMID: 33164754.
Tranexamic acid for ACE inhibitor induced angioedema
Tranexamic acid (TXA) is an antifibrinolytic agent primarily used to manage hereditary angioedema by inhibiting plasminogen activation and bradykinin formation. Although evidence is limited, a case report suggests TXA may also be effective in treating ACE inhibitor-induced angioedema (ACEI-AE), highlighting its potential as a treatment option and the need for further research.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/33164754/.Hasara S, Wilson K, Amatea J, Anderson J. Tranexamic Acid for the Emergency Treatment of Angiotensin-Converting Enzyme Inhibitor-Induced Angioedema. Cureus. 2021 Sep 20;13(9):e18116. doi: 10.7759/cureus.18116. PMID: 34692327; PMCID: PMC8525683.
Tranexamic Acid for the Emergency Treatment of Angiotensin-Converting Enzyme Inhibitor-Induced Angioedema
This study evaluated the use of tranexamic acid (TXA) in managing angiotensin-converting enzyme inhibitor-induced angioedema (ACEi-AE) in the emergency department (ED). Of the 16 patients treated, only 2 required intubation before TXA administration, and none needed intubation afterward, suggesting TXA may be effective in reducing intubation rates. TXA was also associated with a low rate of adverse effects, making it a promising addition to standard care for ACEi-AE.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/34692327/Frank MM, Gelfand JA, Atkinson JP. Hereditary angioedema: the clinical syndrome and its management. Ann Intern Med. 1976 May;84(5):580-93. doi: 10.7326/0003-4819-84-5-580. PMID: 1275365.
Hereditary angioedema: the clinical syndrome and its management
Hereditary angioedema is a genetic condition causing recurrent swelling of the extremities, face, airway, or abdomen, often triggered spontaneously or by trauma. Diagnosis involves detecting low C4 or C1 esterase inhibitor activity, and treatment includes long-term and short-term prophylaxis with antifibrinolytic agents, androgens, or plasma transfusions, as well as supportive care during acute attacks to prevent complications like airway obstruction. Advances in therapy have significantly reduced mortality rates, which were historically as high as 30%.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/1275365/.Ritchie BC. Protease inhibitors in the treatment of hereditary angioedema. Transfus Apher Sci. 2003 Dec;29(3):259-67. doi: 10.1016/j.transci.2003.08.004. PMID: 14572819.
Protease inhibitors in the treatment of hereditary angioedema
C1 Inhibitor deficiency causes uncontrolled complement activation, leading to unpredictable and potentially life-threatening angioedema. While plasma-derived C1 Inhibitor can rapidly treat attacks, it is costly and may not work in cases of autoantibody-mediated angioedema. Antifibrinolytic agents like tranexamic acid are effective for prophylaxis, and novel treatments such as the kallikrein inhibitor DX-88 are under clinical investigation.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/14572819/.Van Sickels NJ, Hunsaker RB, Van Sickels JE. Hereditary angioedema: treatment, management, and precautions in patients presenting for dental care. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010 Feb;109(2):168-72. doi: 10.1016/j.tripleo.2009.09.031. PMID: 20123405.
Hereditary angioedema: treatment, management, and precautions in patients presenting for dental care
Hereditary angioedema (HAE) is a nonhistamine-mediated condition causing tissue edema that does not respond to standard treatments like epinephrine or antihistamines. It is managed with therapies such as tranexamic acid, C1 esterase inhibitors, or fresh-frozen plasma, and airway intervention may be needed in acute cases. Minor trauma or stress can trigger delayed swelling, and angiotensin-converting enzyme inhibitors may worsen symptoms.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/20123405/.Caballero T. Treatment of Hereditary Angioedema. J Investig Allergol Clin Immunol. 2021 Feb;31(1):1-16. doi: 10.18176/jiaci.0653. PMID: 33602658.
Treatment of Hereditary Angioedema
Hereditary angioedema (C1-INH-HAE) is a rare genetic disorder that has seen significant advancements in treatment over the past decade, particularly through targeting the kallikrein-kinin system. Current therapies focus on acute treatment, short-term prophylaxis, and long-term prophylaxis, with several drugs approved for self-administration. Ongoing research is exploring new drugs aimed at blocking the kallikrein-kinin system to improve long-term management of C1-INH-HAE.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/33602658/.\]González JA, Gallart MT, Martí I, Rodrigo MJ. Edema angioneurótico hereditario: estudio del complemento y ensayo terapéutico con ácido tranexámico [Hereditary angioneurotic edema: study of serum complement and therapeutic trial with tranexamic acid (author’s transl)]. Med Clin (Barc). 1980 Jun 10;75(1):10-6. Spanish. PMID: 6993801.
[Hereditary angioneurotic edema: study of serum complement and therapeutic trial with tranexamic acid (author’s transl)]
A study evaluated three familial generations with hereditary angioneurotic edema (HAE), focusing on clinical and immunological factors. The trial with tranexamic acid demonstrated its effectiveness in treating HAE, showing fewer side effects compared to other treatments. The study also highlighted the importance of screening asymptomatic family members to detect low plasma levels of C1-INH.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/6993801/.Kesh S, Singh U, Bernstein JA. Longitudinal experience with treatment of acquired angioedema using tranexamic acid. Allergy Asthma Proc. 2022 Sep 1;43(5):413-418. doi: 10.2500/aap.2022.43.220043. PMID: 36065111.
Longitudinal experience with treatment of acquired angioedema using tranexamic acid
Acquired angioedema (AAE) is a rare condition often linked to lymphoproliferative disorders and anti-C1 esterase inhibitor antibodies, with no standardized treatment. A retrospective review of 13 patients showed that tranexamic acid (TXA) significantly reduced AAE attacks by up to 99% over 24 months, making it an effective prophylactic option. However, adverse effects, such as a deep vein thrombosis in one patient, highlight the need for further treatment alternatives.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/36065111/.Munch EP, Weeke B. Non-hereditary angioedema treated with tranexamic acid. A 6-month placebo controlled trial with follow-up 4 years later. Allergy. 1985 Feb;40(2):92-7. doi: 10.1111/j.1398-9995.1985.tb02666.x. PMID: 3887974.
Non-hereditary angioedema treated with tranexamic acid. A 6-month placebo controlled trial with follow-up 4 years later
A double-blind study treated 10 patients with non-hereditary angioedema using tranexamic acid or placebo for 3 months. Nine patients showed significant improvement with tranexamic acid, while one was unaffected, and side effects like diarrhea and abdominal discomfort occurred in some cases. Four years later, six responders were still using tranexamic acid regularly, with two using it less frequently due to reduced attacks.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/3887974/.Munch EP, Weeke B. Non-hereditary angioedema treated with tranexamic acid. A 6-month placebo controlled trial with follow-up 4 years later. Allergy. 1985 Feb;40(2):92-7. doi: 10.1111/j.1398-9995.1985.tb02666.x. PMID: 3887974.
Non-hereditary angioedema treated with tranexamic acid. A 6-month placebo controlled trial with follow-up 4 years later
In a double-blind study of 10 patients with non-hereditary angioedema, 9 showed significant improvement or became symptom-free with tranexamic acid treatment compared to placebo (P < 0.05), while itching improved in 3 of 4 affected patients. Although diarrhea and abdominal discomfort were more frequent (P < 0.05), only one required a dose reduction. Four years later, 6 of 8 responders continued regular use, while 2 reported infrequent attacks and no longer required consistent treatment.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/3887974/.
Roberts I. Tranexamic acid in trauma: how should we use it? J Thromb Haemost. 2015 Jun;13 Suppl 1:S195-9. doi: 10.1111/jth.12878. PMID: 26149023.
Tranexamic acid in trauma: how should we use it?
Tranexamic acid (TXA) reduces blood loss by preventing fibrin breakdown and is widely used in surgery and trauma care to decrease bleeding and the need for transfusion. The CRASH-2 trial demonstrated that TXA, administered within 3 hours of injury, reduces the risk of death from hemorrhage by about one-third without significant adverse effects, making it suitable for a broad range of bleeding trauma patients. Restricting its use could lead to preventable deaths, and ongoing research, such as the CRASH-3 trial, is exploring its potential benefits in traumatic brain injury.
You can read the full article at https://www.jthjournal.org/article/S1538-7836(22)04212-X/fulltext.
Pabinger I, Fries D, Schöchl H, Streif W, Toller W. Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis. Wien Klin Wochenschr. 2017 May;129(9-10):303-316. doi: 10.1007/s00508-017-1194-y. Epub 2017 Apr 21. PMID: 28432428; PMCID: PMC5429347.
Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis
Uncontrolled massive bleeding, often caused by hyperfibrinolysis (HF), poses a significant challenge in managing surgical and trauma patients, especially those involving organs rich in plasminogen activators. HF leads to excessive bleeding and high mortality, requiring effective intervention. Tranexamic acid (TXA), a synthetic lysine analogue available since 1966, is a crucial antifibrinolytic for preventing and treating HF-related bleeding, reducing perioperative blood loss and transfusion needs. Its applications span various hemorrhagic conditions, with guidelines and research supporting its indications and dosages.
You can read the full article at https://pubmed.ncbi.nlm.nih.gov/28432428/.
McQuilten ZK, Wood EM, Medcalf RL. When to use tranexamic acid for the treatment of major bleeding? J Thromb Haemost. 2024 Mar;22(3):581-593. doi: 10.1016/j.jtha.2023.10.001. Epub 2023 Oct 11. PMID: 37827378.
When to use tranexamic acid for the treatment of major bleeding?
Tranexamic acid (TXA), an antifibrinolytic agent originally developed for postpartum hemorrhage (PPH), has shown efficacy in managing active bleeding across various clinical contexts, with effectiveness influenced by timing, dose, and setting. Early administration is crucial, particularly in trauma and PPH, and while TXA generally does not increase thrombotic risks, it may raise venous thrombosis risk in gastrointestinal bleeding and seizure risk at higher doses. Further research is needed to optimize dosing, administration, and understand its mechanisms in contexts like intracerebral hemorrhage, emphasizing individualized patient assessment and context-specific evidence to improve outcomes.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/37827378/.
Ker K, Mansukhani R, Shakur-Still H, Arribas M, Beaumont D, Roberts I. Tranexamic acid for gastrointestinal bleeding: can a reduction in the risk of death be discounted? A systematic review and meta-analysis of individual patient data from 64 724 bleeding patients. BMJ Open. 2023 Feb 22;13(2):e059982. doi: 10.1136/bmjopen-2021-059982. PMID: 36813490; PMCID: PMC9950890.
Tranexamic acid for gastrointestinal bleeding: can a reduction in the risk of death be discounted?
The HALT-IT trial found no evidence that tranexamic acid (TXA) reduces mortality in gastrointestinal bleeding, but a systematic review and meta-analysis of 64,724 patients across four large trials showed TXA reduces the odds of death by 16% overall and by 20% when administered within 3 hours of bleeding onset, without increasing vascular occlusive events. These findings suggest that the HALT-IT results align with evidence supporting TXA’s efficacy in reducing mortality across various bleeding conditions.
You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC9950890/.
Hunt BJ. The current place of tranexamic acid in the management of bleeding. Anaesthesia. 2015 Jan;70 Suppl 1:50-3, e18. doi: 10.1111/anae.12910. PMID: 25440395.
The current place of tranexamic acid in the management of bleeding
Tranexamic acid has gained significant attention for its ability to reduce morbidity and mortality in surgical and traumatic bleeding. It reduces traumatic bleeding mortality by a third and minimizes blood loss and transfusion needs in surgical patients, with both intravenous and topical applications. While generally safe, high doses may cause neurological side effects without added efficacy, as studies show 1 g intravenously is optimal. The CRASH-2 trial demonstrated no increased thrombotic risk and even reduced myocardial infarction rates, though further research is needed to assess its effects on postoperative venous and arterial thromboembolism in surgical settings.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/25440395/.
VanderMeulen H, Tang GH, Sholzberg M. Tranexamic acid for management of heavy vaginal bleeding: barriers to access and myths surrounding its use. Res Pract Thromb Haemost. 2024 Mar 19;8(3):102389. doi: 10.1016/j.rpth.2024.102389. PMID: 38623473; PMCID: PMC11017359.
Tranexamic acid for management of heavy vaginal bleeding: barriers to access and myths surrounding its use
Tranexamic acid is a safe and effective treatment for heavy menstrual bleeding and postpartum hemorrhage, significantly improving quality of life, reducing mortality risk, and enabling better participation in daily activities. However, its widespread use is hindered by barriers such as structural sexism, period poverty, stigmatization of vaginal blood loss, misinformation in labeling, and limited drug access, which perpetuate inequities in women’s health. The evidence supporting its benefits and the challenges to its utilization were highlighted at the 2023 International Society on Thrombosis and Haemostasis Congress.
You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC11017359/.
Ker K, Edwards P, Perel P, Shakur H, Roberts I. Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis. BMJ. 2012 May 17;344:e3054. doi: 10.1136/bmj.e3054. PMID: 22611164; PMCID: PMC3356857.
Effect of tranexamic acid on surgical bleeding: systematic review and cumulative meta-analysis
This systematic review and meta-analysis of 129 randomized controlled trials involving 10,488 patients found that tranexamic acid significantly reduces the need for blood transfusions in surgical patients by approximately one-third, with strong evidence supporting its efficacy. However, its impact on thromboembolic events (e.g., myocardial infarction, stroke, deep vein thrombosis, and pulmonary embolism) and mortality remains uncertain. While fewer deaths were observed in the tranexamic acid group, the evidence was less robust when restricted to trials with adequate allocation concealment. Further research on its effects on thromboembolic events and mortality is needed, and patients should be informed of these findings to make informed decisions.
You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC3356857/.
Roberts I, Brenner A, Shakur-Still H. Tranexamic acid for bleeding: Much more than a treatment for postpartum hemorrhage. Am J Obstet Gynecol MFM. 2023 Feb;5(2S):100722. doi: 10.1016/j.ajogmf.2022.100722. Epub 2022 Aug 19. PMID: 35988879.
Tranexamic acid for bleeding: Much more than a treatment for postpartum hemorrhage
Early use of tranexamic acid significantly reduces postpartum hemorrhage (PPH) deaths, with major implications for global obstetrical care, particularly in low- and middle-income countries where access is limited. Beyond PPH, tranexamic acid could address maternal anemia by reducing heavy menstrual bleeding, improve blood availability by minimizing surgical blood loss, and lower healthcare costs by reducing transfusions and associated risks. Expanding its use in trauma care could also reduce mortality from violence and injuries. Collaborative efforts to increase access should highlight these broader health benefits to promote its integration across diverse healthcare settings.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/35988879/.
Ockerman A, Vanassche T, Garip M, Vandenbriele C, Engelen MM, Martens J, Politis C, Jacobs R, Verhamme P. Tranexamic acid for the prevention and treatment of bleeding in surgery, trauma and bleeding disorders: a narrative review. Thromb J. 2021 Aug 11;19(1):54. doi: 10.1186/s12959-021-00303-9. PMID: 34380507; PMCID: PMC8356407.
Tranexamic acid for the prevention and treatment of bleeding in surgery, trauma and bleeding disorders: a narrative review
Tranexamic acid (TXA) effectively reduces bleeding in various clinical settings, including surgeries, trauma, and certain bleeding disorders, with strong evidence for its use in menorrhagia, postpartum hemorrhage, and trauma-related mortality reduction. While generally safe, high doses can increase seizure risk in brain injury and cardiac surgery, and delayed administration in trauma or postpartum hemorrhage may raise mortality. Evidence for efficacy in traumatic brain injury and gastrointestinal bleeding is lacking, and thrombotic risks remain a concern in specific scenarios. Ongoing research aims to refine TXA’s optimal dosing and timing to balance its benefits and risks.
You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC8356407/.
Kumar M, Venishetty S, Jindal A, Bihari C, Maiwall R, Vijayaraghavan R, Saggere Muralikrishna S, Arora V, Kumar G, Sarin SK. Tranexamic acid in upper gastrointestinal bleed in patients with cirrhosis: A randomized controlled trial. Hepatology. 2024 Aug 1;80(2):376-388. doi: 10.1097/HEP.0000000000000817. Epub 2024 Mar 5. PMID: 38441903.
Tranexamic acid in upper gastrointestinal bleed in patients with cirrhosis: A randomized controlled trial
In patients with advanced liver cirrhosis (Child-Turcotte-Pugh class B or C) presenting with upper gastrointestinal bleeding (UGIB), tranexamic acid significantly reduced the failure to control bleeding by day 5 (6.3% vs. 13.3%, p=0.006) and failure to prevent rebleeding from esophageal variceal ligation (EVL) sites compared to placebo, though mortality rates at 5 days and 6 weeks were similar between groups.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/38441903/.
Lee PL, Yang KS, Tsai HW, Hou SK, Kang YN, Chang CC. Tranexamic acid for gastrointestinal bleeding: A systematic review with meta-analysis of randomized clinical trials. Am J Emerg Med. 2021 Jul;45:269-279. doi: 10.1016/j.ajem.2020.08.062. Epub 2020 Aug 29. PMID: 33041136.
Tranexamic acid for gastrointestinal bleeding: A systematic review with meta-analysis of randomized clinical trials
This systematic review and meta-analysis of 13 randomized controlled trials (n=2271) demonstrates that tranexamic acid significantly reduces continued bleeding, urgent endoscopic intervention, and mortality in patients with upper gastrointestinal bleeding, supporting its use in emergency settings. However, its effects on lower gastrointestinal bleeding remain unclear and require further investigation.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/33041136/.
Dunn CJ, Goa KL. Tranexamic acid: a review of its use in surgery and other indications. Drugs. 1999 Jun;57(6):1005-32. doi: 10.2165/00003495-199957060-00017. PMID: 10400410.
Tranexamic acid: a review of its use in surgery and other indications
Tranexamic acid, a synthetic lysine derivative, effectively reduces blood loss and transfusion needs in various surgeries, including cardiac, oral, and liver procedures, and shows efficacy in treating upper gastrointestinal bleeding, menorrhagia, and pregnancy-related bleeding. It demonstrates comparable or superior benefits to other antifibrinolytics, such as aprotinin, with a favorable safety profile and no increased thrombosis risk in clinical trials.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/10400410/.
Dionne JC, Oczkowski SJW, Hunt BJ, Antonelli M, Wijnberge M, Raasveld SJ, Vlaar APJ; for ESICM Transfusion Taskforce and the GUIDE Group. Tranexamic Acid in Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis. Crit Care Med. 2022 Mar 1;50(3):e313-e319. doi: 10.1097/CCM.0000000000005362. PMID: 34709209.
Tranexamic Acid in Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis
The study evaluated the efficacy and safety of tranexamic acid (TXA) in gastrointestinal bleeding through a systematic review and meta-analysis of randomized controlled trials. Extended-use high-dose IV TXA did not reduce mortality or bleeding and was associated with an increased risk of adverse events, including deep venous thrombosis, pulmonary embolism, and seizures. In contrast, low-dose IV or enteral TXA showed moderate evidence of reducing rebleeding and the need for surgery without improving mortality, highlighting the need for further research to confirm its safety and efficacy.
You can read the abstract of this article at https://pubmed.ncbi.nlm.nih.gov/34709209/.
Lukes AS, Moore KA, Muse KN, Gersten JK, Hecht BR, Edlund M, Richter HE, Eder SE, Attia GR, Patrick DL, Rubin A, Shangold GA. Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol. 2010 Oct;116(4):865-875. doi: 10.1097/AOG.0b013e3181f20177. PMID: 20859150.
Tranexamic acid treatment for heavy menstrual bleeding: a randomized controlled trial
This double-blind, placebo-controlled study demonstrated that oral tranexamic acid (3.9 g/day) significantly reduced menstrual blood loss and improved health-related quality of life in women with heavy menstrual bleeding. Over six cycles, tranexamic acid achieved a 40.4% reduction in menstrual blood loss compared to 8.2% with placebo, meeting all primary efficacy endpoints. Women treated with tranexamic acid reported meaningful improvements in physical, social, and work activities, with most adverse events being mild to moderate and similar in frequency to placebo.
You can read the abstract at https://pubmed.ncbi.nlm.nih.gov/20859150/.
- Cai J, Ribkoff J, Olson S, Raghunathan V, Al-Samkari H, DeLoughery TG, Shatzel JJ. The many roles of tranexamic acid: An overview of the clinical indications for TXA in medical and surgical patients. Eur J Haematol. 2020 Feb;104(2):79-87. doi: 10.1111/ejh.13348. Epub 2019 Dec 16. PMID: 31729076; PMCID: PMC7023891.
- The many roles of tranexamic acid: An overview of the clinical indications for TXA in medical and surgical patientsTranexamic acid (TXA) is a widely researched antifibrinolytic agent effective in managing bleeding from surgery, trauma, obstetric complications, and various hemostatic disorders. Its established roles in postpartum hemorrhage, menorrhagia, trauma-related bleeding, and surgical bleeding are complemented by emerging evidence of broader applications, demonstrating its ability to reduce bleeding and improve outcomes without significantly increasing thrombotic risk.
You can read the full article at https://pmc.ncbi.nlm.nih.gov/articles/PMC7023891/.
Other Peptides
Patient Success Stories

Before
After

At the age of 60, I look and feel better than I ever have in my entire life! Switching my health program and hormone replacement therapy regimen over to Genemedics was one of the best decisions I’ve ever made in my life! Genemedics and Dr George have significantly improved my quality of life and also dramatically improved my overall health.
Nick Cassavetes ,60 yrs old Movie Director (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer

Before
After

I am now in my mid-sixties and feel better than I did in my 20’s. Many people have commented that I actually look 20 years younger since I started the program at Genemedics. Calling Dr. George has proven to be one of the best decisions I have made in my life. Doctors and society convince us that developing various health issues and negative sy...
Pamela Hill ,66 yrs old Actress (“The Notebook”, “John Q”, “Alpha Dog”), Actor and Writer
What to expect during your consultation:
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have
Free Consultation
Start Your Journey to a Younger, Healthier You!
Categories
Information
Free Consultation
STEPS AWAY FROM A YOUNGER. HEALTHIER YOU!
Call 800-277-4041 for a Free Consultation
What to expect during your consultation:
- Usually takes 15-30 minutes
- Completely confidential
- No obligation to purchase anything
- We will discuss your symptoms along with your health and fitness goals
- Free post-consult access for any additional questions you may have